Overlooked Adverse Reactions: Gastrointestinal Symptoms
Are GI symptoms post-vaccination a possible predictor of circulating spike protein and other downstream effects?
I know I promised viral parkinsonism as my next topic, but given the prior posts associating SARS-COV2 with gut dysbiosis, I was curious about whether the vaccines may be associated with GI issues themselves.
The hypothesis surrounding gut dysbiosis and microbiome alterations propose 2 possibilities:
ACEII receptors are widespread among many of the cells in the gut, and therefore it’s quite possible that SARS-COV2 may infect these cells and lead to negative alterations in the gut.
Systemic inflammation and the circulation of various cytokines may also lead to gut alterations, as the gastrointestinal tract is sensitive to inflammatory markers.
Although I lean a bit more towards the second argument, the first one shouldn’t be discounted, because what the first hypothesis would point towards would be further indication of circulating spike.
That is, if vaccinees experience GI issues then we may infer some relationship to spike binding to ACEII receptors in the gut, causing downstream effects akin to those seen with the virus.
It would also be a rather obvious symptom to recognize relative to more severe symptoms as myocarditis, blood clots, and other serious complications may not be recognized until far too late.
So I tried perusing a few studies to see if there have been any indication of widespread diarrhea and stomach pains.
GI symptoms post-vaccination
The information has been, unfortunately, rather sparse and may be reflective of the limited information regarding a lack of data collection with respect to vaccine adverse reactions.
One of a select few studies on the matter comes from Lee, et al.1 which looked at retrospective information from a select clinic in Seoul, South Korea from the time period of March 1, 2021 - July 30, 2021.
Here, patients (46) who visited the ED (emergency department) for digestive issues post-vaccination were considered for the study.
Patients included those who were given both mRNA and adenoviral vaccines, with digestive symptoms generally occurring within a day of vaccination and usually occurring with the first dose of the vaccine:
COVID-19 vaccines from three different brands were used; 33 patients received AZD1222 (AstraZeneca), nine received BNT162b2 (Pfizer/BioNTech), and three received JNJ-78436735 (Johnson and Johnson). The median time for the onset of digestive symptoms after vaccination was 1 (1,1) days. Most digestive symptoms appeared following the administration of the first dose of the vaccine. Comorbidities included hypertension, diabetes mellitus, chronic obstructive pulmonary disease, and musculoskeletal disease (Table 1).
When it comes to digestive symptoms researchers noted several different symptoms including diarrhea, blood in the stool (hematochezia), as well as darkened stool (melena) in a select few patients:
In total, 14 (30%) patients experienced digestive symptoms only (Table 2 ). These included abdominal pain, diarrhea, dyspepsia, nausea, hematochezia, and melena. Patients (70%) experienced additional symptoms, including fever and poor oral intake (Table 2). Abdominal pain, diarrhea, fever, and inadequate oral intake were frequently observed in severe cases.

Given that some of these symptoms are also seen in those with COVID, the researchers point to an interesting description called “Vaccine-Induced COVID-19 Mimicry”.
Because of these shared symptoms, it would make sense that these may be associated with the common structure found in both SARS-COV2 and the vaccines, which is the spike protein.
Thus, the prominence of these symptoms may be suggestive of circulating spike, which may bind to ACEII receptors within the gut and lead to gut dysbiosis and other GI issues. However, it should be noted that the effect of the spikes within the gut would warrant movement of the spike from the blood into the gut environment.
How this would occur should be brought into question, however it appears that many of the symptoms were more frequently and more severe in those with comorbidities.
As several comorbidities have been related to gut dysbiosis and gut permeability, it can be argued that spike may translocate from the blood into the gut, akin to bacteria translocating into the blood and causing bacteremia.
Effects from a strong inflammatory response should also not be overlooked given that systemic inflammation may also alter the gut microbiome and may be another explanation for these GI issues.
It’s interesting that diarrhea appears more prominently in those with more mild cases of COVID, which raises some questions as to whether GI symptoms may be related more to the inflammatory response rather than the virus.
Aside from the Lee, et al. study the information on adverse reactions are rather sparse.
One case report from Ajmera, et al.2 notes a case of a 41-year old Caucasian male who received a Moderna booster and began experiencing diarrhea and increasing abdominal pain the following morning, leading him to go to the ER:
Our patient was a 41-year-old Caucasian male with a past medical history of bipolar depression, asthma, and obesity (body mass index: 40 kg/m2) who presented to the emergency room (ER) with the chief complaint of abdominal pain. The patient had received a Moderna COVID-19 vaccine booster dose the day prior to presentation to the ER. On the morning of the day of presentation to the ER, the patient started experiencing diarrhea and progressively worsening sharp, intermittent, generalized abdominal pain associated with sweating and loss of appetite. The patient rated intensity at 5 out of 10.
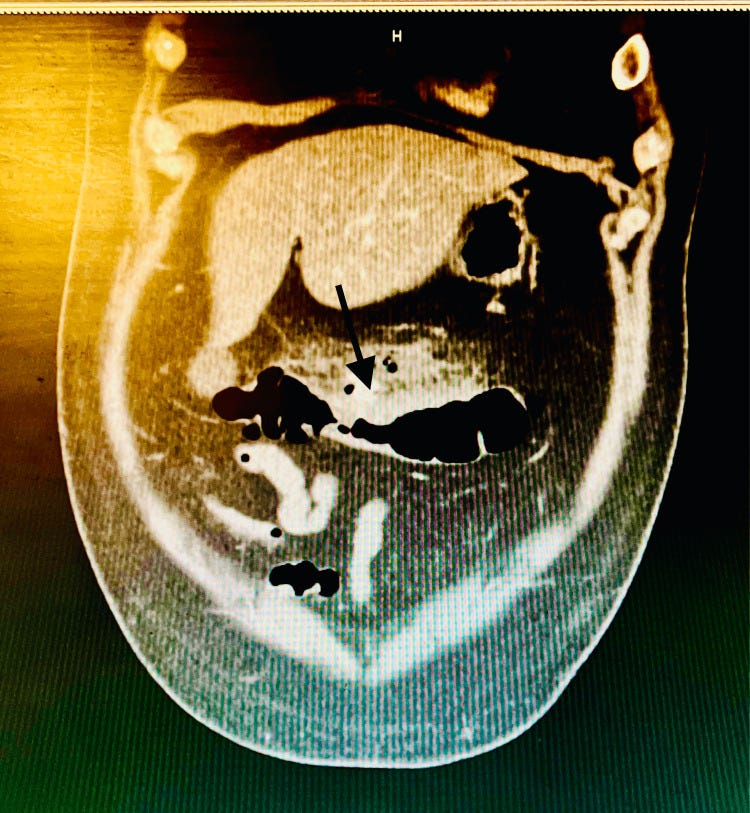
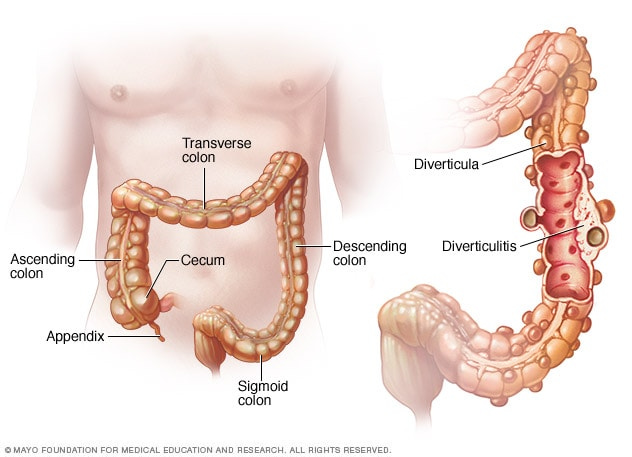
An abdomen CT scan was recommended, which noted possible perforation of acute diverticulitis: inflammation of diverticula3 (small pouches commonly found within the large intestines, predominately the colon).
General surgery consult was obtained for further evaluation. Upon their recommendation, a CT scan of the abdomen with IV and oral contrast was obtained, which re-demonstrated stranding around the transverse colon, concerning for acute diverticulitis. Within this region, there remained a few areas of extraluminal air and fluid without a discrete drainable abscess, consistent with viscus perforation. However, imaging did not reveal any active leakage of the contrast, suggesting a sealed-off perforation, hence did not necessitate emergent surgical intervention (Figure 1).
The hypothesis raised by the researchers are similar to those of Lee, et al. and the vaccine-induced mimicry:
Our hypothesis is that transcribed viral spike protein binds to cells in the GI tract in a manner similar to that of the actual virus, promoting dysbiosis and inflammation. Hence, the vaccine is able to produce various GI symptoms in recipients, similar to patients infected with SARS-CoV-2. However, this hypothesis needs to be further explored in clinical trials.
In another case report from Akaishi, et al.4 a 46-year old woman with no prior evidence of gastrointestinal disease reported prolonged diarrhea and vomiting months after receiving her second dose of the Pfizer-BioNTech vaccine, although she had symptoms following her first dose as well:
A 46-year-old woman with no notable medical history developed repeated vomiting approximately four hours after receiving the first BNT162b2 mRNA COVID-19 vaccine. After 2 days, she felt pain at the injection site, which resolved within several days. Seven days after the first vaccination, she further developed 3-5 loose-to-liquid stools per day, which corresponded to type 6 on the Bristol Stool Form (BSF) Scale (Lewis and Heaton 1997). Before vaccination, she had no significant gastrointestinal (GI) problems and had a normal bowel pattern and stool formation. Two weeks after the first vaccine dose, intermittent paraumbilical pain developed with associated loss of appetite. Although the patient was anxious about receiving the second vaccine dose, she decided to receive the second dose 21 days after the first dose. After 7 days, vomiting and diarrhea progressed, with 7-10 watery stools per day (BSF type 7). The symptoms did not alleviate with time, and she gradually felt difficulty in oral intake.
Testing did not find anything abnormal, but 28 weeks post the patient’s 2nd dose she presented to the hospital with a fever, diarrhea and bloody stools.
She was diagnosed with gastroenteritis and hemorrhoids5, and at the time of the article’s publication her symptoms did not resolve (around 32 weeks after her 2nd dose).
A timeline provided by Akaishi, et al. notes symptom onset and treatment:
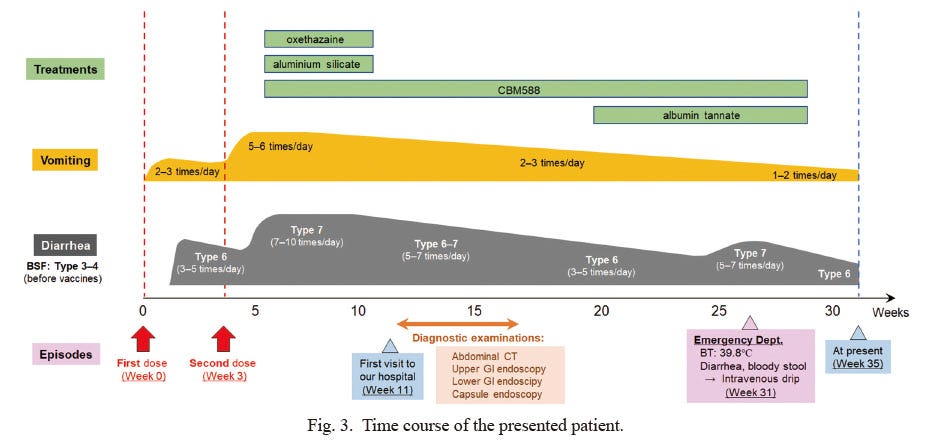
The case of the woman presented above is an unfortunate, severe case detailing longterm GI issues post-vaccination that did not appear to resolve at the time of the publication.
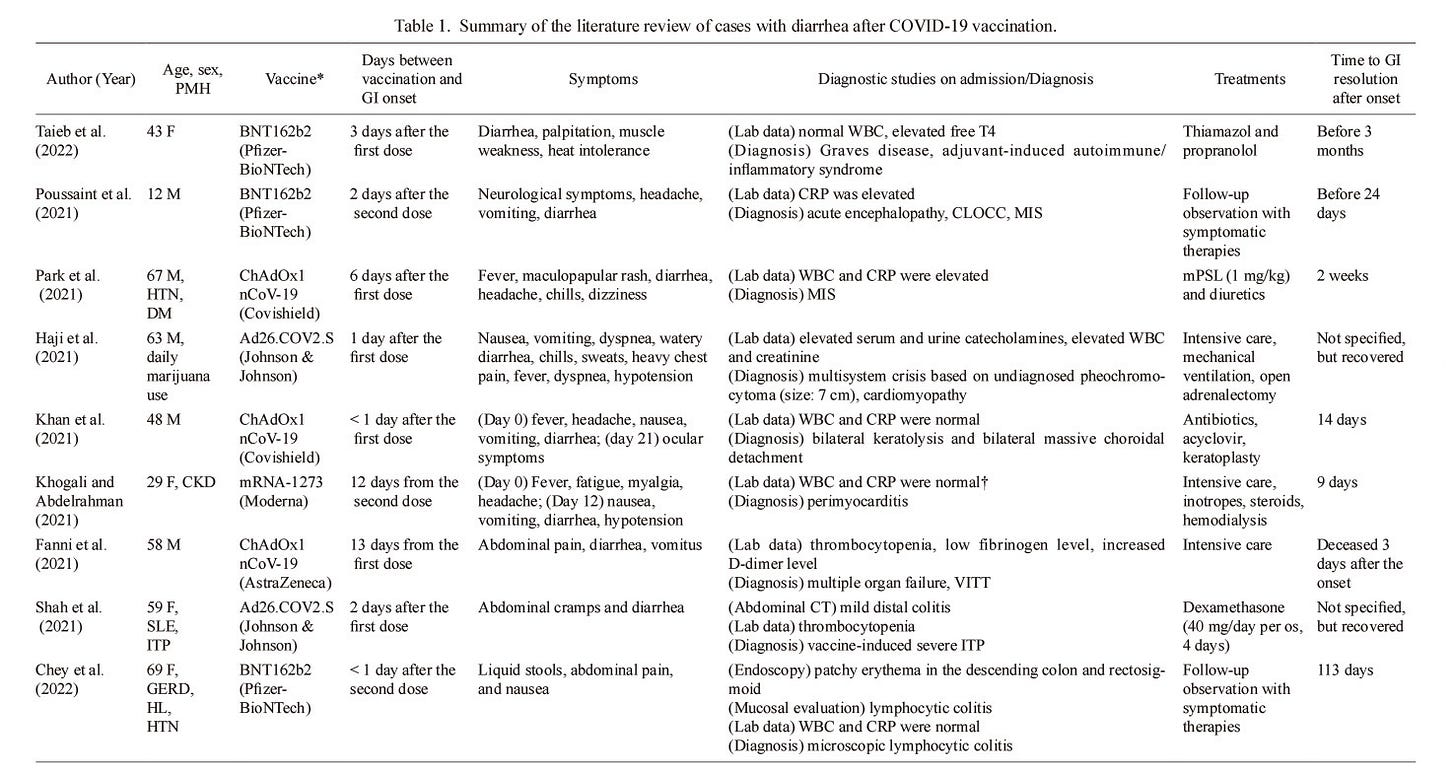
In order to find additional information on other evidence of GI issues Akaishi, et al. conducted a literature review noting any studies in which GI issues were noted post-vaccination which includes vaccines from various platforms:
The researchers note that several accounts, including VAERS, suggests around a 3% reported incidence of diarrhea. Although rather small, scaling up and accounting for underreporting may suggest a possible high number of vaccinees who have experienced (and may continue to be experiencing) GI issues.
One hypothesis proposed by Akaishi, et al. suggests, once again, a possible association between SARS-COV2’s spike and gut dysbiosis:
The most probable explanation for the GI symptoms observed in the present case could be the occurrence of gut dysbiosis after COVID-19 vaccination. The importance of gut microbiota in the immune response against the invasion of external pathogens through both the respiratory and GI tracts is widely known (Wu and Wu 2012). In patients with COVID-19, the microbiota of the respiratory and GI tracts have been shown to be dramatically altered after infection (Wang et al. 2022). The fecal microbiomes of patients with COVID-19 are deficient in beneficial anti-inflammatory symbionts, such as Eubacterium, Lachnospiraceae, and Faecalibacterium, and are abundant in opportunistic microbes, such as Clostridium spp., Enterobacteriaceae, Enterococcus, and Bacteroides spp. (Zuo et al. 2020). Gut dysbiosis often persists even after recovery from COVID-19 and clearance of the virus (Yeoh et al. 2021). This fact strongly supports the theory that gut dysbiosis and the subsequent immunological disequilibrium triggered by COVID-19 infection or vaccines may contribute to persistent GI symptoms that last for more than several months. In addition to patients with COVID-19, vaccinees also have altered gut microbiota (Ng et al. 2022). Such post-vaccine gut dysbiosis may play a crucial role in the development of persistent GI symptoms in some vaccinees.
Overall, the limited evidence points to a possible role in spike-associated gut dysbiosis post-vaccination.
It’s important to note that this effect doesn’t appear to be related to just the mRNA and adenoviral vector vaccines as some evidence suggests that GI symptoms have been seen in inactivated and subunit vaccines.6 This would add further evidence to the possibility of spike-related GI dysbiosis akin to that seen with a SARS-COV2 infection.
GI Symptoms as Possible Predictor?
When looking at all of these reports on adverse reactions or of people “dying suddenly”, I became more concerned with the ease of use for this phrase because it tends to gloss over a lot of nuance.
Let’s take for instance someone who dies of a heart attack. The moment the heart attack occurs may be sudden, and hence we may argue that it may appear that someone may have “died suddenly”.
But what if the lead-up to the heart attack was preceded with headaches, nausea, and difficulty breathing for several weeks. Would we then consider the heart attack to have been sudden, or would we argue that some context clues should have alerted us to the possibility of heart attack?
The problem is that the use of the phrase “died suddenly” suggests that there would be nothing to look for when in reality there may be clues to the possibility of an event occurring.
It’s similar to neighbors or friends who make remark that “they were surprised” or were “so shocked” when someone they know commits an atrocity. Although they may play naïve, they may have just bothered to not look for the right things—they weren’t paying attention.
So in some regards I rebuke the widespread use of “died suddenly”, and instead offer a look into signs that may be indicative of severe adverse reactions.
Note that this doesn’t apply to all circumstances. It’s very true that several cases of adverse reactions are acute, in which case the events would not be predictable.
But in cases where they are it’s important to note symptoms and what these symptoms may be associated with.
Here, we looked at a possible underexamined adverse reaction from COVID vaccination: GI issues.
Several reports have noted that the onset of diarrhea and vomiting usually appear the following day, and usually occur after the 1st dose.
Remember in the Yonker, et al.7 piece a comment was made that the 1st dose of the vaccine may lead to circulating S1 subunits of spike which should be cleared (hypothetically speaking) after the second dose due to antibody binding:
It has previously been shown that after the first inocula-tion of the mRNA-1273 vaccine, the cleaved S1 sub-unit of spike can be detected in the plasma of healthy adults.16 However, after the second dose, no antigen was detected,16 presumably because there are higher levels of circulating anti–SARS-CoV-2 antibodies, which quickly bind any circulating antigen, facilitating its clearance.
This remark should be taken with some skepticism without additional context, but this may allude to the fact that the neophyte immune response may not be able to deal with the spike protein being produced, causing them to circulate and find their way into the gut and causing the symptoms of diarrhea and indigestion.
This may suggest that GI symptoms may serve as a possible predictor of other adverse reactions as they may note circulating spike. However, this prediction may be rather poor given that many adverse reactions seem to increase with every additional dose.
This also doesn’t tell us if the initial immune response mounted can adequately remove the spike, and this comes on the heels of information suggesting Pfizer may not even know what proteins the vaccines are producing!
This effect may also indicate the importance of the microbiome. As gut dysbiosis may lead to permeability it’s possible that circulating spike may gain better access to the gut of those who have limited biodiversity.
On one hand a poor microbiome may suggest more severe GI symptoms post-vaccination and from COVID, while a diverse, proper microbiome may attenuate some of these adverse reactions and be associated with improved outcomes.
More studies would be needed to validate this association, but it’s worth considering whether GI issues may provide a sign of what’s going on in the body.
Now, just to get a little more…personal, let’s take a few polls!
I suppose it’d be nice to see who had any GI symptoms during COVID, as well as those who may have experienced GI symptoms after vaccines, or know of people who have.
Note that these polls are anonymous so you aren’t giving out identifying information.
Again, this is anonymous and done more to get a wild, very unscientific guesstimate of some people’s experiences.
The next post will take a look at hypertension post-vaccine. A warning that the data here will be limited as well, but I will try to make do with what I can find.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

Lee, D. S., Kim, J. W., Lee, K. L., Jung, Y. J., & Kang, H. W. (2022). Significance of digestive symptoms after COVID-19 vaccination: A retrospective single-center study. The American journal of emergency medicine, 58, 154–158. https://doi.org/10.1016/j.ajem.2022.05.044
Ajmera, K., Bansal, R., Wilkinson, H., & Goyal, L. (2022). Gastrointestinal Complications of COVID-19 Vaccines. Cureus, 14(4), e24070. https://doi.org/10.7759/cureus.24070
The Mayo Clinic provides an image of these diverticula. It’s noted that they are common, usually appearing in prominence as one gets older.
Akaishi, T., Takahashi, T., Sato, S., Jin, X., Masamune, A., & Ishii, T. (2022). Prolonged Diarrhea Following COVID-19 Vaccination: A Case Report and Literature Review. The Tohoku journal of experimental medicine, 257(3), 251–259. https://doi.org/10.1620/tjem.2022.J043
The researchers note a non-specific inflammatory response given the staining and slides of colonic mucosa.
Dadras, O., Mehraeen, E., Karimi, A., Tantuoyir, M. M., Afzalian, A., Nazarian, N., Mojdeganlou, H., Mirzapour, P., Shamsabadi, A., Dashti, M., Ghasemzadeh, A., Vahedi, F., Shobeiri, P., Pashaei, Z., & SeyedAlinaghi, S. (2022). Safety and Adverse Events Related to Inactivated COVID-19 Vaccines and Novavax;a Systematic Review. Archives of academic emergency medicine, 10(1), e54. https://doi.org/10.22037/aaem.v10i1.1585
Yonker, L. M., Swank, Z., Bartsch, Y. C., Burns, M. D., Kane, A., Boribong, B. P., Davis, J. P., Loiselle, M., Novak, T., Senussi, Y., Cheng, C. A., Burgess, E., Edlow, A. G., Chou, J., Dionne, A., Balaguru, D., Lahoud-Rahme, M., Arditi, M., Julg, B., Randolph, A. G., … Walt, D. R. (2023). Circulating Spike Protein Detected in Post-COVID-19 mRNA Vaccine Myocarditis. Circulation, 10.1161/CIRCULATIONAHA.122.061025. Advance online publication. https://doi.org/10.1161/CIRCULATIONAHA.122.061025


That first Korean study that you used- did they differentiate the cases between the 4 different types of jabs?
I got omicron and no gastro issues (but i felt awful like when i had dengue fever). My son also had omicron, no gastro (sinuses were runny and he had a fever and a headache). When he had to get J and j for college a year before his omicron, he had only a fever- it was terrible, 105.3 degrees, i thought the thermometer was broken. I had to put him in a cold bath for 4 hours with advil and tylenol to get it down to 103.
Thank you for this article. I am curious if you have seen any studies or information about Covid and Covid vaccines in those with Celiac. I have Celiac and my GI system was definitely impacted both times I got Covid.