Circulating spike in post-vaccinated adolescents
Free, uncleaved spike were found in the blood of some adolescents with myocarditis, possibly alluding to an age-related adverse reaction.
Several weeks ago a study was published in Circulation1, a journal of the American Heart Association, in which researchers compared immunological profiles of adolescents who experienced post-COVID vaccine myocarditis compared to those who were asymptomatic.
Several people have reported on this article before (apologies for not remembering who!), and so I shelved it for the time being.
However, it’s worth pointing out a few parts of this study that stood out and may explain the higher prevalence of myocarditis in adolescent males compared to adults.
The study enrolled 61 adolescents/young adults between the ages of 12-21 between January 2021 and February 2022.
This included 16 people with recorded post-vaccine myocarditis and 45 asymptomatic cases. However, after age-matching and limiting the time window following vaccination to 11 days the number of participants were actually 10 and 17, respectively.
A layout of the study can be seen below, but remember that the cohorts are actually 10 post-vaccine myocarditis compared to 17 asymptomatic control.

It’s worth pointing out that the paper uses the language of “asymptomatic” for their control group, and that’s unfortunately due to a selection bias here.
Participants were recruited based on presentation of symptoms at either Massachusetts General Hospital (MGH) or Boston Children's Hospital (BCH).2
In contrast, asymptomatic participants were recruited from local clinics or from referrals within 3 weeks post-vaccination, with these people commenting on not having noted any chest pains or requiring treatment post-vaccination.3
This creates a few problems, because asymptomatic does not inherently mean myocarditis-free. It’s plausible that one may have damaged heart or organs without really experiencing any symptoms, hence why the language here uses “asymptomatic” rather than “myocarditis-free” or words similar to that, as no tests were done to indicate that no adverse reactions had occurred in either group.
The time difference is also an issue, as the researchers noted that symptoms of myocarditis were usually within a week of vaccination. The myocarditis cohort had a median time of 4 days post-vaccination4, while the median time for the controls were 14 days, a rather big difference. The cutoff for 11 days also suggests that many of the asymptomatic participants were over the cutoff period, and with the earliest timepoint in the asymptomatic cohort apparently being 4 days it does raise questions as to how many participants were near the cutoff period in the control cohort, although that’s speculation on my part.
The language of the paper also appears to suggest that any myocarditis cases in 1-dose and boosted participants were likely excluded.
In any case, the lack of relative time matching means that any immunological profiles that occur days onward may be far different than the ones early on and may not capture the actual scope of the events. The time delay may be reflected in the troponin levels, but again we’re having to speculate here.
Key Findings
As several people have looked at this study I will focus on the aspects that stood out.
Inflammatory markers were elevated in post-myocarditis participants
When researchers compared cytokine profiles of myocarditis participants to controls, they noted that cytokine levels were elevated:
Although minimal differences were seen in the T-cell populations, individuals with myocarditis displayed dis-tinct cytokine profiles reminiscent of the profile seen in MIS-C,17–19 suggesting likely innate inflammatory activa-tion, with significantly elevated levels of interleukin (IL)-8, IL-6, tumor necrosis factor-α, IL-10, interferon-γ, and I L- 1β and lower IL-4 levels compared with healthy vac-cinated control subjects (Figure 3A–3G) with no notable differences in IL-5, IL-12p70, or IL-22 (Figure 3H–3K).
Comparison of cytokine profiles should be done with hesitancy over outliers, which appear quite often in the following data. However, clearly elevated levels of IL-6 can be noted, with IL-4 being noticeably lower in myocarditis participants (boxed below).

Edit 4/20/2023: The caption originally stated that IL-4 was lower in the control group when it should have stated that it was lower in the myocarditis group. It has been corrected in the italics above.
Production of IL-4 comes largely from T-cells5, and so it’s interesting that the researchers comment that T-cell profiles were similar between groups (likely owed to the very small sample size, as can be seen in Supplementary Figure 2), and yet IL-4 production was higher in control groups. However, IL-4 is also produced by mast cells, eosinophils, and basophils, and so the lack of profiling of other immune cells may have been a factor.
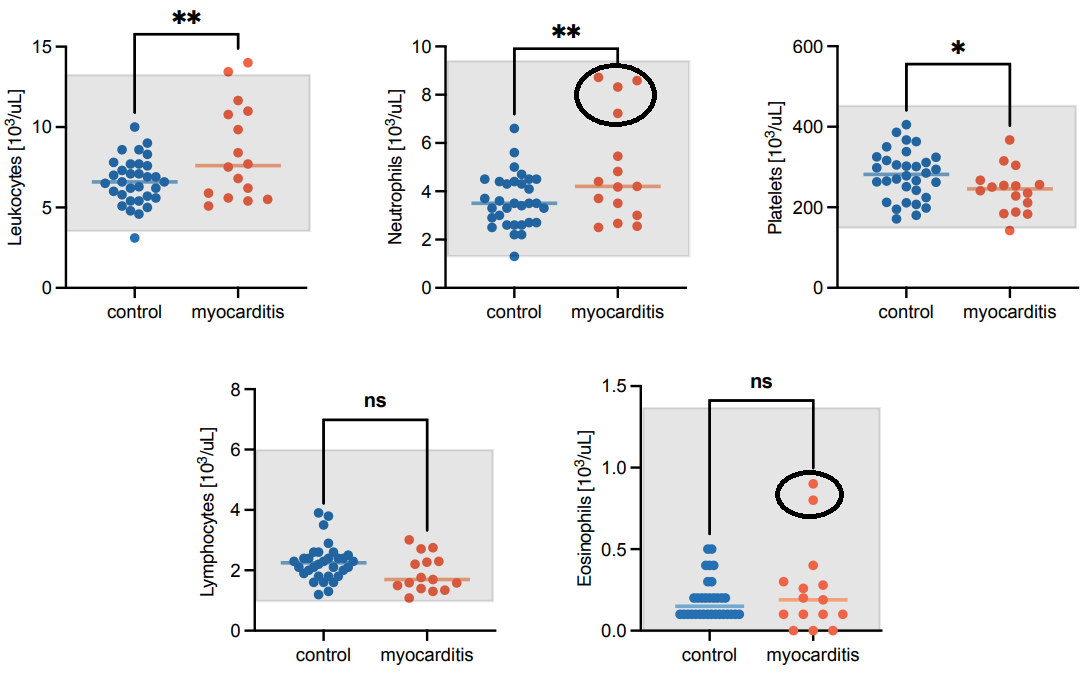
The researchers note that neutrophils were elevated in myocarditis participants, however there are also outlier factors for both neutrophil and eosinophil measures (circled below):
Taken altogether, the elevated cytokine levels in myocarditis patients are interesting. The overall evidence suggest innate immune activation may be elevated in myocarditis patients, however, the evidence comes with limitations.
Free, unbound, uncleaved spike in myocarditis participants
Probably one of the most interesting findings comes from the type of spike that was collected.
Here, researchers looked at both full spike and the S1 subunit and examined their quantity in blood. Researchers also looked at antibody-bound spike and S1 subunits as well.
Interestingly, the researchers noted that that there were higher levels of free, unbound, and uncleaved spike in myocarditis patients when compared to control participants:

I’ve thrown around a few terms, but if we dissect it using the figure above we can expand more on these points:
Again, note that “bound” here is being inferred based on the difference in free and total. Free spike or S1 subunits were easily detected through the assays used. However, treatment (with DTT) was needed to remove the bound antibodies and expose the spike or subunits in order to quantify them, noted in the top image of Figure 4. Therefore, dots in the “total” column but none in the “free” column would suggest these antigens were bound by antibodies.
With that, many S1 subunits were found to be bound to antibodies in control participants whereas very few were noted in the myocarditis group (comparing the values in the left table). It’s important to note that S1 appeared to be cleared more frequently in adults relative to younger participants.
In contrast, full spike was noted more in the myocarditis group relative to the control group (graph on the right). Most of the spike was unbound, as the free and total values appear comparable (the orange dots on on the right chart).
When comparing the two charts it becomes apparent that the myocarditis group had higher levels of free, unbound, and uncleaved spike compared to the control group who had predominately bound S1 subunits (comparing the dots in chart 1 to chart 2, where all of the dots were noted in “control, total” on the left and the dots were noted in the “free, myocarditis" on the right.
These findings are significant due to their “strangeness”.
The researchers note that most spike detected in adults were S1 subunits:
It has previously been shown that after the first inocula-tion of the mRNA-1273 vaccine, the cleaved S1 sub-unit of spike can be detected in the plasma of healthy adults.16 However, after the second dose, no antigen was detected,16 presumably because there are higher levels of circulating anti–SARS-CoV-2 antibodies, which quickly bind any circulating antigen, facilitating its clearance.
This is important, because it suggests a possible difference in spike processing between age groups, wherein the inability to cleave the spike may be related to something immunological or something related to expression of TMPRSS2.
But this may also be due to something not extensively looked at, in that the immune response in younger people are biased towards innate immunity.
It’s been suggested that one of the reasons why children fare better with COVID may be due to a stronger innate immunity. Although innate immunity is not all that matters, in the presence of a novel virus having a stronger innate immune system may be more beneficial as a first line of defense, and thus younger people with a stronger innate immune system may fare better.
However, in the context of vaccination it may be that the presentation of the antigen by one’s own cells may not adequately dealt with when confronted with a predominately innate immune response. It’s possible here that the body’s attempt to deal with the spike may not adequately encapsulate the spike in antibodies, or lead to an adaptive immune response akin to adults as would occur with an adaptive response.
*Edit 4/18/2023: Antigens was changed to antibodies in the paragraph above, and is indicated in italics.
Therefore the spike, unprocessed and unbound, may roam freely in younger individuals and lead to the adverse reactions seen.
As it relates to TMPRSS2, there’s insufficient evidence looking at age-related TMPRSS2 expression.
However, several therapeutics have been looked at in targeting this enzyme in order to protect against COVID.
Interestingly, one mutation in TMPRSS2 called rs12329760 alters a valine-160 residue to methionine. It’s been suggested that the enzyme expressing methionine has poorer cleavage capacity and syncytium formation, and may provide a genetic explanation for why some people fare better, especially those homozygous for this mutation.6
This mutation is, interestingly enough, seen in East Asian populations,7 and may explain their better outcomes during the early years of COVID. However, as Omicron moved more towards endosomal entry into cells TMPRSS2 became less necessary.
It'd be interesting to see if the outbreaks in China and other places in East Asia may be owed to Omicron not needing TMPRSS2 for viral entry, and thus a removal of this genetic protection.
But much of that may be besides the point. What’s critical here is that for some reason the spike antigen doesn’t appear to be readily cleaved by younger individuals to the same degree as adults, and it could be that this inability to process spike, possibly due to a bias towards an innate immune response or age-related expression of TMPRSS2, may explain why young men may be experiencing higher rates of myocarditis.
For further thought
The concept of “spike in the blood” is no longer novel. It’s quite apparent that the components of the vaccine do not confide themselves to the local area of injection.
However, what this study sheds light on is the fact that the entire process leading to spike entering into the blood should be looked into.
That is to say, what exactly happens to the spike and how it is dealt with is also critical.
Here, it appears that those who experienced myocarditis had an elevated innate immune response.
However, given that innate immunity seems to be one of the key components of protection in children, it begs the question of what exactly is going on here.
It’s quite possible that the presentation of antigen is what’s key, as unlike typical viral infections where the antigen can clearly be seen as an exogenous substance, here the use of host cells to produce spike may actually be creating a precarious scenario in how the spike is dealt with as the cascade of events may actually differ to a significant degree.
But much of this is speculative. More studies should see confirm the dominance of free spike in myocarditis patients, as well as the role that the innate immune system plays in vaccination. Is it inherently beneficial, or could an innate immune response actually be detrimental in the dealing with the spike?
More importantly, it’s quite possible that the response in children will be far different than adults, and therefore requires further investigation.
Hopefully additional insights will come out to piece together this discrepancy.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

Yonker, L. M., Swank, Z., Bartsch, Y. C., Burns, M. D., Kane, A., Boribong, B. P., Davis, J. P., Loiselle, M., Novak, T., Senussi, Y., Cheng, C. A., Burgess, E., Edlow, A. G., Chou, J., Dionne, A., Balaguru, D., Lahoud-Rahme, M., Arditi, M., Julg, B., Randolph, A. G., … Walt, D. R. (2023). Circulating Spike Protein Detected in Post-COVID-19 mRNA Vaccine Myocarditis. Circulation, 10.1161/CIRCULATIONAHA.122.061025. Advance online publication. https://doi.org/10.1161/CIRCULATIONAHA.122.061025
The Supplementary Material makes note that the post-vaccine myocarditis participants were admitted to the following hospitals.
Adolescents and young adults presenting with chest pain and elevated cardiac troponin T levels after recent SARS-CoV-2 mRNA vaccination, who were admitted to the pediatric wards or the pediatric intensive care units at the Massachusetts General Hospital (MGH) or Boston Children’s Hospital (BCH), were approached to enroll in the Institutional Review Board (IRB)- approved Pediatric COVID-19 Biorepository at MGH 14 (Mass General Brigham IRB #2020P0000955) or the IRB-approved “Taking on COVID-19 Together” Biorepository at BCH (BCH IRB #P00035409). Both biorepositories were established to collect samples from children during the COVID-19 pandemic to understand the impact of SARS-CoV-2 on children
A convenience sample of healthy controls, who were recruited from local pediatric clinics and referrals, included age-matched adolescents and young adults who received their second SARS-CoV-2 mRNA vaccination within the past three weeks. Healthy controls denied any chest pain and did not require any medical attention following vaccination. Informed consent, and assent when applicable, was obtained from participants and/or parents/guardians prior to enrollment of these individuals in the Pediatric COVID-19 Biorepository at MGH.
Note that a median timepoint of 4 days suggests that nearly half of the reported myocarditis cases occurred nearly right after vaccination and suggests a rather acute response.
Brown, M. A., & Hural, J. (2017). Functions of IL-4 and Control of Its Expression. Critical reviews in immunology, 37(2-6), 181–212. https://doi.org/10.1615/CritRevImmunol.v37.i2-6.30
Beheshti Shirazi, S. S., Sakhaee, F., Sotoodehnejadnematalahi, F., Zamani, M. S., Ahmadi, I., Anvari, E., & Fateh, A. (2022). rs12329760 Polymorphism in Transmembrane Serine Protease 2 Gene and Risk of Coronavirus Disease 2019 Mortality. BioMed research international, 2022, 7841969. https://doi.org/10.1155/2022/7841969
Sekiya, T., Ogura, Y., Kai, H., Kawaguchi, A., Okawa, S., Hirohama, M., Kuroki, T., Morii, W., Hara, A., Hiramatsu, Y., Hitomi, S., Kawakami, Y., Arakawa, Y., Maruo, K., Chiba, S., Suzuki, H., Kojima, H., Tachikawa, H., & Yamagata, K. (2022). TMPRSS2 gene polymorphism common in East Asians confers decreased COVID-19 susceptibility. Frontiers in microbiology, 13, 943877. https://doi.org/10.3389/fmicb.2022.943877





I thought the mRNA vaccines encoded the prefusion spike that was locked in place and stable against cleavage? It was shocking to see that high levels of S1 were reported. If I'm not mistaken, S1 is much more pathogenic than full spike.
With every passing day I am more and more thankful that I didn't inject my kids.