HHV-related Meningitis/Encephalitis following COVID Vaccination
Case reports of brain inflammation associated with HHV reactivation post-vaccination.
Prior posts for those interested:
Following the prior posts this one will be shorter in nature (apologies for the rather long posts!). As has been discussed previously there is clear evidence of HHV reactivation in those who were infected with SARS-COV2 as well as in those who were vaccinated.
In these cases recognition of HHV reactivation, and usually VZV in particular, is done by way of looking for cutaneous signs/symptoms of reactivation. That is, a rash and blisters following vaccination is likely a presentation of VZV reactivation as herpes zoster (shingles).
However, not all HHV reactivations may represent with cutaneous symptoms. Remember the two cases reports from Bookhout, et al.1 in which two fatal cases of otherwise treatable HHV infections went unnoticed until too late, with one person not presenting with cutaneous symptoms until far too late into the disease while the other individual never presented with cutaneous symptoms. Therefore, cutaneous symptoms may not be the best method of discerning HHV reactivation, and certainly may prove deadly if not recognized by other means.
This is emphasized by the fact that cognitive impairment post-COVID and post-vaccination has been widely reported, as well as growing evidence and recognition of parallels between HHV reactivation and Long COVID.
With that in mind, the following is intended to introduce case reports in which neurological complications, predominately meningitis and encephalitis due to HHV reactivation, have been noted post-COVID vaccination, emphasizing the point that a lot of serious adverse events may be overlooked or unrecognized.
Encephalitis vs Meningitis
Before we begin, we should note that some of these case reports will either note encephalitis or meningitis in these individuals.
As the -itis suffix implies, both are diseases of inflammation, and in particular both note inflammation of the CNS. However, meningitis refers predominately to inflammation of the meninges, which are 3 layers of membranes that envelop the spinal chord and the skull (all recognized by the word mater).
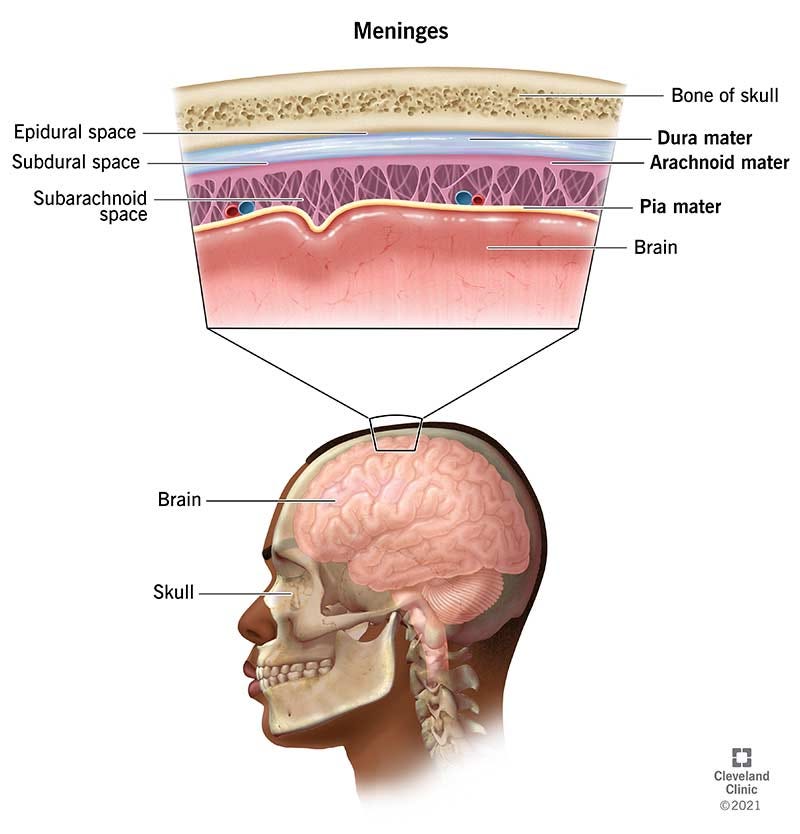
In contrast, encephalitis refers to inflammation of the brain itself.2
Both forms of inflammation can be caused by infectious agents including viral agents such as HHVs which tend to show neurotropism.
The signs and symptoms for both encephalitis and meningitis overlap and may even appear flu-like, although more severe forms of inflammation may present more differently. One contrasting symptom is that meningitis may present as neck stiffness.
Some of the signs and symptoms for each inflammation can be seen below (both from the NIH website):
Encephalitis Signs/Symptoms
Meningitis Signs/Symptoms
Post-Vaccination Case reports
Again, there may be a bit of disorganization here, but when possible distinctions will be made for the type of vaccine, what dose, and strain of HHV if detected.
Encephalitis Post-Vaccination
One case report from Moslemi, et al.3 notes of a 27-year old man who awoke to sudden vomiting 3 days after receiving the first dose of the Oxford/AstraZeneca adenoviral vaccine. He began experiencing severe headaches and changes in mental faculties, eventually ending up in the ER after worsening symptoms. Preliminary diagnosis suggested possible encephalitis, and eventual suspicion of herpetic encephalitis led to the use of Acyclovir for the patient. Meanwhile, most lab tests appeared normal with no neurological deficits recognized.
The authors don’t appear to mention evidence of cutaneous symptoms.
CFS samples noted the presence of Herpes Simplex 1 viral DNA, confirming the suspicion of herpetic encephalitis. The patient was prescribed Acyclovir for 21 days, and although he didn’t make a full recovery by the time of discharge he showed visible improvements.
This is one of the first reported cases of possible HSV1 reactivation following COVID vaccination. As the authors imply, lack of treatment can become devastating for the patient. Unfortunately, the lack of evidence in the literature suggests that many clinicians may not be aware of considering this association, or how to treat such an event.
This appears to be one of the only cases of herpetic encephalitis following COVID vaccination, although there has been reported cases of encephalitis following vaccination that appear to be associated with other factors such as possible autoimmunity, suggesting that manifestation of encephalopathy may be due to other factors but relating to a commonality of the COVID vaccines.
Meningitis Post-Vaccination
Unlike herpetic encephalitis, there appears to be some evidence of meningitis associated with HHV reactivation following vaccination.
One of the first case reports recorded in the literature is from Maruki, et al.4 in which case a 71-year old woman with IgA nephritis began experiencing headaches the day after receiving the first dose of the Pfizer/BioNTech vaccine. She had a stiff neck although no neurological complications.
However, 5 days after her vaccination she began experiencing painful erythematous (red) patches, leading to a diagnosis of possible VZV-related meningitis which was confirmed with lesion sample testing and CSF PCR testing for VZV DNA.
Although this patient presented with cutaneous signs of VZV reactivation, the presentation was localized and rather minimal, in which case such presentation may be easily missed. This patient was also recognized as being immunocompetent, and thus also raises a question of possible VZV-reactivation following a vaccination as this may imply a possible window of immune deficiency as has been suggested previously.
In one case report from Medhat, et al.5 a 46-year old woman presented to the clinic with 3 days of severe headaches which did not respond to treatments. The patient’s COVID vaccine history included prior vaccination with two doses of Sinopharm’s inactivated virus vaccines, along with a booster dose of Pfizer/BioNTech’s vaccine 3 weeks prior to the onset of the headaches.
The patient presented as hypotensive and with a low-grade fever, with the only other notable symptom being neck stiffness.
A lumbar puncture would later come back positive for VZV from PCR, suggesting VZV-related meningitis which was later confirmed with another VZV PCR test (not based on CSF).
The patient was administered many different medications, but the focus became Acyclovir after the positive PCR test leading to eventual full recovery.
Although the authors suggest a possible vaccine-related case of VZV meningitis, note that the onset of the meningitis occurred weeks post-vaccination, and so some hesitancy may be warranted in making such an immediate conclusion. Also, note that this case occurred with the mRNA booster after inactivated virus vaccines, and so presents with an interesting case. Given that HHV reactivation has a higher prevalence with the Pfizer/BioNTech vaccine this may infer something related to this vaccine in particular that is worth considering, although this comes with the caveat that the Pfizer/BioNTech vaccine was administered at a much higher rate than the others.
A report from Buranasakda, et al.6 notes two cases in which VZV meningitis occurred within 10 days of receiving different COVID vaccines.
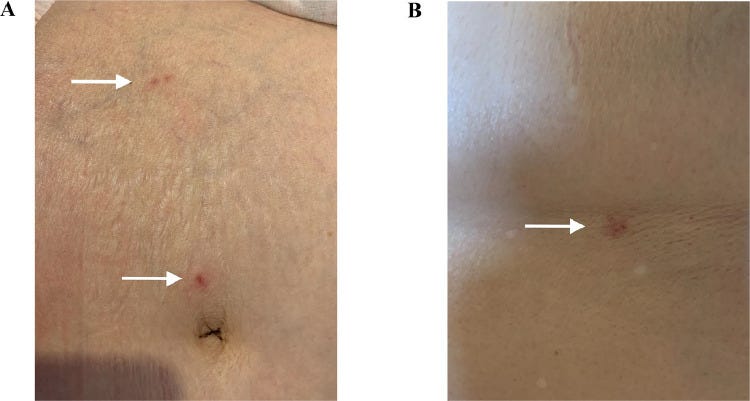
One patient, a 34-year old man with a history of being infected with VZV twice during childhood, presented with lesions along the left side of his waist 5 days after receiving the first dose of the inactivated virus vaccine from Sinovac. Nine days after vaccination the patient presented to the clinic with severe headaches. The patient would go on to present with a stiff neck along with more lesions along his back.
Eventual PCR tests would turn up positive for VZV, leading to a diagnosis of VZV meningitis. The patient was administered Acyclovir intravenously for 14 days and appeared to make a full recovery. The patient would later go on to receive AstraZeneca’s vaccine with no apparent evidence of an adverse event.
In contrast, the second case notes of a 32-year old man who began experiencing headaches 5 days after receiving the first dose of the AstraZeneca vaccine.
Upon initial presentation the patient did not have any skin lesions. A lumbar puncture was conducted on this patient as well.
Two days after admission the patient was reported has having lesions on his back, and CSF PCR would eventually come up positive for VZV, suggesting VZV meningitis. The patient was also placed on a 14-day regimen of Acyclovir.
In the end, the patient seemed to have full resolution of symptoms and went on to receive the second dose of the AstraZeneca vaccine one month later, noting a mild fever afterwards.
Note the contrast in these two cases. Not only did these two patients receive different vaccines, but one presented with cutaneous symptoms prior to the onset of headaches while the other had headaches that preceded the skin lesions, again suggesting that some patients may not have recognizable lesions or ashes but an otherwise viral-related episode of meningitis.
Things to Consider
The reported cases of either meningitis or encephalitis relating to the COVID vaccines have so far been very limited. This may be due to underreporting or not contributing these events to vaccines. At the same time, like with all HHV reactivations, it’s important to consider that many factors can contribute to HHV reactivation, and so any reemergence of shingles may also be associated with some risk of meningitis or encephalitis. It’s quite possible that some of these events are coincidental.
With that being said, what’s also important within the context of the COVID vaccines is the fact that it seems rather evident that they contribute in some way to the ability for HHVs to become reactivated.
This may either be due to immunomodulatory properties of vaccines, or it could be due to factors related to the spike protein. Consider that prior evidence notes that COVID can lead to lymphocytopenia, and so lymphocyte exhaustion, as well as autoimmune responses towards antiviral interferons, may make HHV reactivation more easy relative to prior vaccines.
Therefore, the fact that cutaneous symptoms of HHV reactivation have occurred rather commonly should raise some critical concerns over whether these reactivations may be leading to other diseases. This is worth examining given that these brain inflammations may not present with cutaneous signs but may nonetheless prove deadly if not treated.
Overall, keep in mind that the intent of examining HHV-related adverse events is not to suggest that this is the main culprit for everything going on but something worth considering within the grand scheme of vaccine-related complications.
With that being said, consilience and further remarks will be saved for a future post.
Substack is my main source of income and all support helps to support me in my daily life. If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists such as myself to provide work outside of the mainstream narrative.

Bookhout, C., Moylan, V., & Thorne, L. B. (2016). Two fatal herpesvirus cases: Treatable but easily missed diagnoses. IDCases, 6, 65–67. https://doi.org/10.1016/j.idcr.2016.09.013
Myelitis is inflammation of the spinal chord, and the both of them together (inflammation of both brain and spinal chord) is referred to as encephalomyelitis.
Moslemi, M., Ardalan, M., Haramshahi, M. et al. Herpes simplex encephalitis following ChAdOx1 nCoV-19 vaccination: a case report and review of the literature. BMC Infect Dis 22, 217 (2022). https://doi.org/10.1186/s12879-022-07186-9
Maruki, T., Ishikane, M., Suzuki, T., Ujiie, M., Katano, H., & Ohmagari, N. (2021). A case of varicella zoster virus meningitis following BNT162b2 mRNA COVID-19 vaccination in an immunocompetent patient. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases, 113, 55–57. https://doi.org/10.1016/j.ijid.2021.09.055
Medhat, R., El Lababidi, R., Abdelsalam, M., & Nusair, A. (2022). Varicella-Zoster Virus (VZV) Meningitis in an Immunocompetent Adult after BNT162b2 mRNA COVID-19 Vaccination: A Case Report. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases, 119, 184–186. https://doi.org/10.1016/j.ijid.2022.04.001
Buranasakda, M., Kotruchin, P., Phanthachai, K., Mootsikapun, P., & Chetchotisakd, P. (2022). Varicella zoster meningitis following COVID-19 vaccination: a report of two cases. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases, 119, 214–216. https://doi.org/10.1016/j.ijid.2022.03.055







And the pediatrician still offered the shot to my 14-yr-old yesterday.