Does the type of anti-hypertensive treatment for the vaccine injured matter?
If The Spike Effect is to be considered a valid hypothesis, should the hypertensive treatment used be aimed to counter this effect?
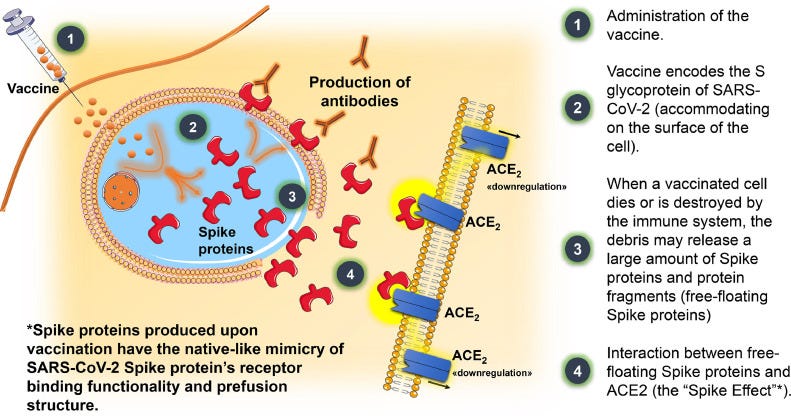
*Cover image from Health Jade
The following is an attempt to suggest a possible method of dealing with hypertension post-vaccination in the form of describing how the type of antihypertensive medication prescribed may have to deal with The Spike Effect. Please note that the following is intended to serve as a hypothetical and not intended to be medical advice. For those experiencing hypertension post-vaccination please consult with a physician and discuss the proper course of treatment for yourself. Again, this is intended to serve as food for thought and something for researchers to consider investigating.
In writing my previous posts on hypertension related to the COVID vaccines I was surprised to find out the number of different blood pressure medications out there.
Interesting, given that in most cases the actual cause of hypertension may not be known. This type of hypertension, known as primary or essential hypertension makes up a majority of all hypertension diagnoses, in which case the hypertension is of unknown etiology. Few cases of hypertension are related to another medical condition; a case of hypertension known as secondary hypertension.
So the main cause of most cases of hypertension is generally unknown, and yet the medications used have different mechanisms of action. This raises questions as to whether people may be receiving improper treatment, and it may explain why blood pressure may be difficult to manage with blood pressure medications alone.
But let’s suppose we take a look at hypertension post-vaccination. Here the direct link of spike to hypertension isn’t fully clear, as it may be the spike working indirectly on various systems to cause hypertension, or it’s possible that spike can act directly on the circulatory system.
The latter effect is what has been referred to as The Spike Effect.
Although mentioned in previous posts, the spike effect is outlined below in the figure from Angeli, et al. 20221
To expand upon this point the following series of events may follow after #4 listed above:
The spike protein may act as a competitive inhibitor, in which it competes with Ang II for binding to ACEII. This may lead to increased serum Ang II levels as Ang II does not get enzymatically cleaved into Ang-(1-7).
Downregulation of ACEII expression may also occur, leading to reduced ACEII and elevated Ang II as well (a two-fold effect).
Elevated Ang II levels would lead to increased binding to AT1R, and this activation leads to pro-inflammatory, pro-oxidative stress, and hypertensive responses from the body.
Here, the end result of The Spike Effect may be long-term activation of AT1R and hypertension, with the end-stage effects possibly being a stroke or heart attack. In this case, it’s reasonable to examine hypertension as a secondary form of hypertension with a possible cause being tied to the spike protein produced by the vaccine.
Again, all of this, so far, is a supposition that relies on limited data due to the lack of research into these adverse reactions, but if we are to entertain the idea of The Spike Effect it would appear that the key factors are Ang II and AT1R.
And it’s because of these two factors that the antihypertensive treatment in question becomes critical.
That’s because different antihypertensives have different mechanisms of action.
The antihypertensives in question here are ones related directly to the renin-angiontensin system, with two classes in particular that target RAS:
ACE Inhibitors: ACE is involved with the conversion of Angiotensin I into Angiotensin II. ACE inhibitors, therefore, block ACE and therefore prevent the production of Ang II.
ACE Inhibitors generally have the suffix “-pril” such as Lisinopril and Enalapril.
Angiotensin Receptor Blockers: Instead of blocking the production of Ang II one can stop the binding of Ang II to AT1R and thus stop the signaling cascade and activation.
ARBs end with “-sartan” such as Candesartan and Losartan
These two classes of drugs have been considered rather contentious in the COVID era, and their use was questioned due to their ability to possibly upregulate ACEII expression.
This raised concerns over whether hypertensive patients who take ACE Inhibitors or ARBs may be at greater risk of severe COVID, or if the use of these medications may help to restore RAS homeostasis that may be perturbed by ACEII downregulation.
Some clinicians even raised questions as to whether patients on ACE inhibitors or ARBs should switch to other antihypertensives.
An article from July 20202 raises some of these points:
Some investigator groups have suggested that ACE inhibitors may be a logical choice for all patients with COVID-19 infection [7]. This is irrespective if patients have pre-existing hypertension or not. The rationale for giving ACE inhibitors to all patients is that it may enhance the expression of ACE2 receptors that further reduce cellular inflammation [2, 7]. There is limited evidence that ACE inhibitors or angiotensin II type 1 receptor blockers (ARB’s) may up-regulate ACE2 receptor mRNA and or expression [2].
Importantly, the COVID-19 infection effectively down-regulates the ACE2 receptor via attaching to infection-related transcription factors at the ACE2 regulatory regions [2]. ANG II also reduces the expression of the ACE2 receptor. Cardiac, lung, liver and renal damage is responsible for morbidity and mortality in COVID-19 [8]. These organ systems have a higher expression of ACE2 receptors than other bodily systems. Because ACE2 converts Ang II to Ang [1,2,3,4,5,6,7], down-regulation of the ACE2 receptor would leave critical organ systems susceptible to hyper-inflammation via unopposed increases in Angiotensin II (ANG II) [2]. Respiratory distress in COVID-19 and SARS is likely associated with reduced ACE2 receptor expression [2, 7,8,9]. Individuals with diabetes, high blood pressure, metabolic syndrome and advanced age (with reduced organ ACE2 expression) are prone to higher fatality rates [10].
As mentioned above, there doesn’t appear to be evidence of ACEII upregulation through the use of both ACE inhibitors and ARBs, which suggest that the use of such drugs likely won’t compensate for ACEII downregulation from the spike.
However, it’s not necessarily the upregulation of ACEII that may be necessary in attenuating The Spike Effect, but the blocking of increasing Ang II that may be critical.
That is to say, would use of ACE inhibitors and ARBs help attenuate hypertension in those who are vaccine injured and hypertensive?
From a very loose, hypothetical perspective it may make sense to argue that attenuation of Ang II buildup may help reduce hypertension, if it is the Ang II and activation of AT1R that is critical in the pathology of the disease.
In cases where other antihypertensive treatments are ineffective, especially when paired with reduced sodium intake, it may be possible to get angiotensin levels checked as noted by The Cleveland Clinic:
Angiotensin is an essential hormone for blood pressure regulation. If you’re having a difficult time maintaining healthy blood pressure and also have changes in your sodium (salt) levels, you may want to talk to your healthcare provider about your angiotensin levels. They can order some tests to see if irregular levels are causing your symptoms.
Thus, for those who are vaccine injured and experiencing hypertension post-vaccination it may be worth discussing with a healthcare provider and see whether angiotensin levels are in order. Irregularities with elevated Ang II levels may point to a possibility of The Spike Effect at play, however it’s possible that the adrenergic system and other factors may the result of elevated Ang II levels.
There’s also the fact that such an effect is contingent on circulating spike. We are still unsure of the longevity of circulating spike (again, lack of studies being conducted), and so it is unknown if persistent hypertension may still be related to spike protein, and even then remember that the spike protein has to be unbound by antibodies to elicit such an effect.
And that comes with the fact that we do not know how many people may have experienced hypertension post-vaccination, and continue to, OR even how many people who “died suddenly” may have died because of unrecognized hypertension as a consequence of the vaccine.
Altogether, The Spike Effect requires several layers evidence to argue its significance. However, for those who are vaccine injured it’s worth considering what exactly may be causing the hypertension, and whether something can be done to deal with it.
Again, remember that this post is meant to serve as food for thought more than to serve as anything prescriptive. Note that the focus of this post was on antihypertensive medications. Another post will be saved for looking at different, non-pharmaceutical options in treating hypertension.
For those who are vaccine injured, or even those who are hypertensive who may not have their blood pressure under control, consult your physician and see what other avenues are possible for you.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

Angeli, F., Zappa, M., Reboldi, G., Gentile, G., Trapasso, M., Spanevello, A., & Verdecchia, P. (2022). The spike effect of acute respiratory syndrome coronavirus 2 and coronavirus disease 2019 vaccines on blood pressure. European journal of internal medicine, S0953-6205(22)00433-2. Advance online publication. https://doi.org/10.1016/j.ejim.2022.12.004
McLachlan, C.S. The angiotensin-converting enzyme 2 (ACE2) receptor in the prevention and treatment of COVID-19 are distinctly different paradigms. Clin Hypertens 26, 14 (2020). https://doi.org/10.1186/s40885-020-00147-x


Terrific article! I am keeping it.
Thank you!!!