The possible relationship between COVID vaccines and other synergistic factors in elevated Catecholamine levels
Part I: Examining the teenager autopsy report for possible leads.
Cadegiani provides a very interesting framework to discuss Catecholamines within the context of mRNA vaccines. However, it is rather limited in scope and doesn’t address the myocarditis issue occurring across all vaccine platforms, indicating that something else may be afoot.
There is this one comment made by Cadeginai that I find very interesting:
It is unlikely that the enhanced catecholamine release, response, receptor sensitivity, and overall activity acted alone to provoke the vaccine-induced, catecholamine-triggered myocardial complications. The catecholamines possibly acted synergistically with other dysfunctions, including abnormal immunological and inflammatory responses, as they alone may cause myocarditis only during extreme catecholamine exposure.
This quote is important because it argues that additional context should be considered when examining myocarditis associated with these vaccines. It’s certainly the case for athletes and higher levels of androgens playing a role in Catecholamine levels. More generally speaking the hypercatecholaminergic state may be caused by other factors that work together to cause the eventual myocarditis and sudden cardiac death.
In one of Stephanie Brail’s recent posts I made this remark in regards to a comment made by someone who had several friends in their 70s suddenly die post-vaccination:
I don't think we should throw out the ideas of lockdowns, but look at the totality of the evidence. There's plenty of factors that work together in order to worsen the situation. I'm working on a post on Catecholamines right now but my Part III will be delayed because I am going down a few rabbit holes. One thing we should consider is that the vaccines should not be considered in isolation i.e. are there variables within certain demographics that turn no adverse events into a case of myocarditis? I think we need to be careful in quickly assuming people are healthy. The case of the older people dying found in the comment of Campbell's video is harrowing, but for people in their 70's how likely are they to have a fully clean bill of health?
I think a few people may have misinterpreted my response here, since I wasn’t saying that the vaccines are not to blame. Rather, I was trying to argue that it’s the culmination of various factors that we need to take into consideration. A 70-year old isn’t quite young and may be on multiple medications. They may suffer from health complications such as obesity, diabetes, osteoporosis, and other possible diseases that may each work collectively to cause the eventually sudden death post-vaccination. There’s certainly no way to know what the context is for these deaths as these appear to have come from Youtube comments, but without context it removes information that may be vital to figuring out what exactly is going on.
Put in another way, think of our bodies as undergoing constant insults on a daily basis either through environmental toxins, consumption of processed foods, constant sitting and even the occasional venture onto Twitter. For the most part our bodies are able to deal with these daily insults (well, maybe not ones from Twitter…), but under some circumstances we may be bombarded with even more insults, or one extremely large insult that, taken altogether, overwhelms our bodies. And it’s within this context that the vaccines should be examined, and it’s what Cadegiani remarks in the above excerpt.
So it was Cadegiani’s remark that spurred me to look a little further into a few of the case reports and see if there were any variables that may be associated with catecholamines and a hyperadrenergic state.
The autopsy of the two adolescent males
In February a widely circulated autopsy report1 came out describing the death of two teenage males who were recently vaccinated. These two boys died in their sleep, and the coroner’s report suggest catecholamine-mediated cardiomyopathy in both instances as being the main culprit for the heart damage. It was here where I first heard of the catecholamine association, as reader Judith Gustafson was the one who provided me with the autopsy report and asked if I could look into it.
Given my limitations in pathology I noted that I wouldn’t be able to look too deeply into the study, but what did catch my eye was the profile of the children.
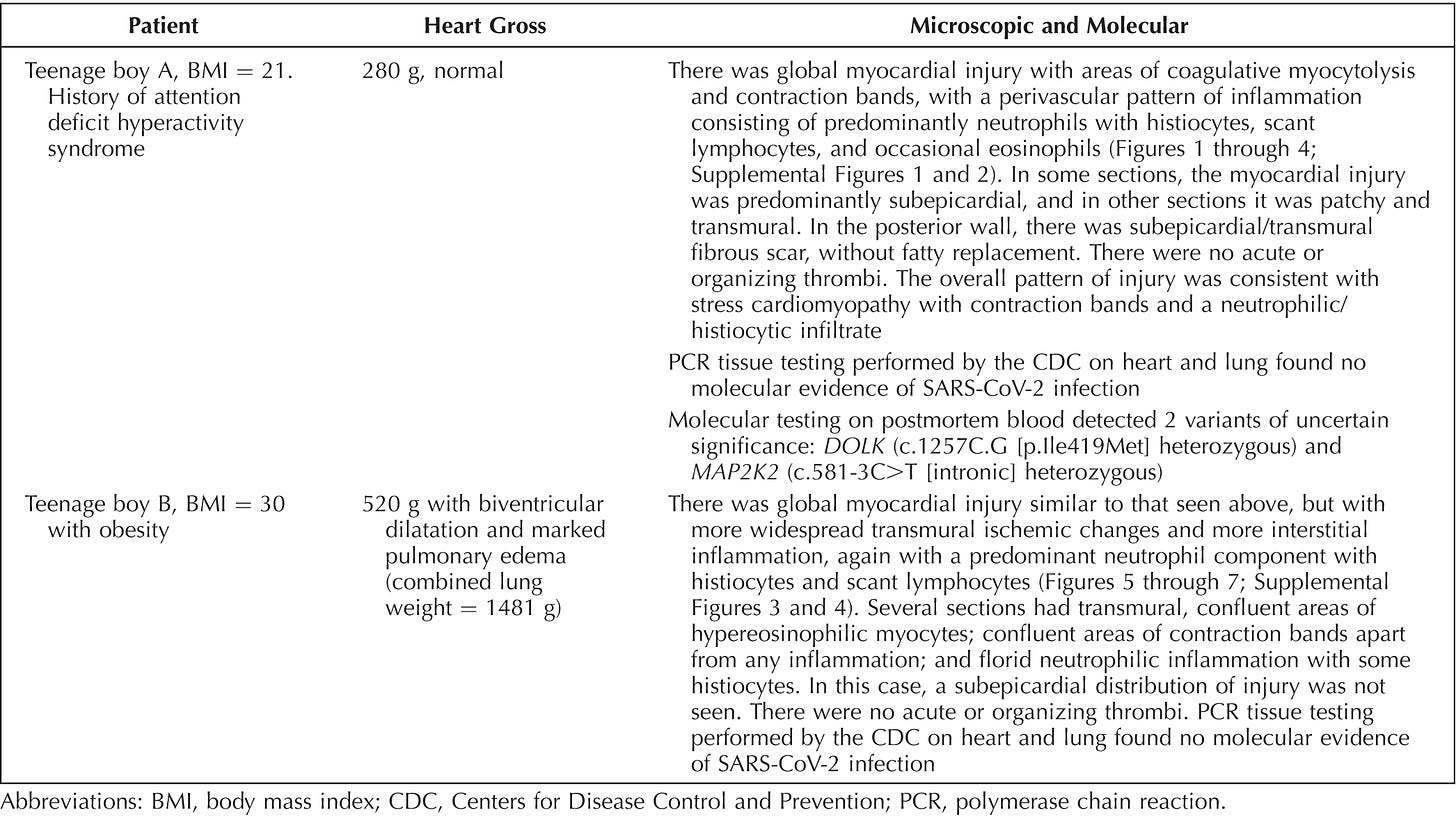
For instance, teenage boy A appeared to have been on Amphetamines for ADHD while teenage boy B was obese (BMI of 30). Some of the findings from the autopsy can be seen below, although I am focusing more on the patient information.
At the time I commented to Judith about these factors (the ADHD and the BMI) but didn’t think much of it, and several people who reported this study made proclamations to the “healthy” status of these teenagers.
However, I should have known better than to ignore other variables at the time. We’ll see why there’s more to this story, and why these seemingly innocuous factors should be worth examining.
Teenager A: the possible association between ADHD and Catecholamines
In the first autopsy report teenager A is reported to have had ADHD. The information provided by the coroner also suggests that he was on medications for his ADHD. Most notably, amphetamines (emphasis mine):
Boy A complained of a headache and gastric upset but felt better by postvaccine day 3. There was no history of prior medical problems (he took prescribed amphetamine/dextroamphetamine during the school year for attention deficit hyperactivity disorder but was not currently receiving it) or prior SARS-CoV-2 infection.
ADHD is short for attention deficit hyperactivity disorder. ADHD is a rather common neurological disorder, usually characterized by an inability to stay focused, feeling a need to move around and not stay still, or possible issues with remembering things. It may usually present in a manner that causes distractions or inattentiveness at school which is where most cases of ADHD may first be noticed. For many children ADHD may be more of a manageable disorder rather than one that can be fully treated, as many children diagnosed with ADHD will have it carry into their adulthoods.
The CDC has an outline of some of these symptoms:
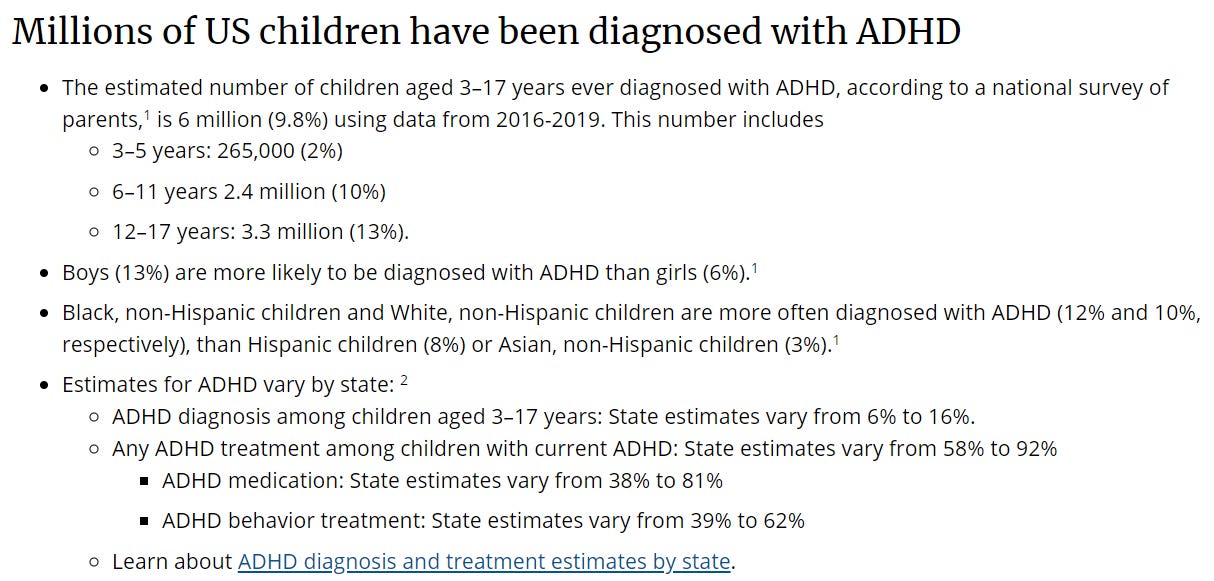
Diagnoses of ADHD have been growing in recent years, and recent data suggests that up to 10% of US teenagers may have been diagnosed with ADHD at some point in their life, as can be seen by the following data provided by the CDC. It’s important to note that ADHD diagnoses heavily skew male:
Now, the etiology/cause of ADHD is rather interesting.
So far there have been no conclusive theories. Several initial thoughts suggested a reduction in grey and white matter within the brain of those with ADHD while others suggested dysfunctions in connectivity with various parts of the brain. More specifically, the regions of the brain called the prefrontal cortex (PFC), medulla and caudate interact with one another through neurotransmitters, and it’s assumed that dysfunction in neurotransmitters and connectivity may be to blame.
Some of these neurotransmitters include Dopamine and Norepinephrine, which led some researchers to assume that ADHD may be associated with Catecholamine dysfunction.
However, this explanation itself is conflicting, as some studies have suggested that ADHD may be caused by either a hypoactive Catecholamine system or a hyperactive one.
In the case of hypoactive systems, a few studies have indicated that reduced Dopamine receptor density and disruption of α receptor function have been implicated in ADHD. However, genetic mutations that increase the influx of Dopamine have also been considered as mechanisms leading to ADHD (i.e. a hyperactive system).
The evidence is conflicting, but it appears that ADHD may be caused by either too little Catecholamines or too many Catecholamines, suggesting that a moderate balance may be key in reducing symptoms of ADHD (Sharma, A. & Couture, J.2):
The hypoactive and hyperactive catecholamine hypotheses of ADHD have been integrated by the facts that DA and NE may exhibit an inverted U-shaped dose-response curve9 similar to that observed with vitamins, where either extreme is a problem and that 2 separate pools of DA14 and NE25 exist in the brain (Figure 1). An appropriate level of DA/NE is required for optimal functioning of the PFC, and disruption leads to ADHD. Medications helpful in ADHD restore the delicate balance of the NTs in the PFC and are discussed later. However, a correct diagnosis of ADHD must precede prescription of these drugs to avoid exposing unaffected individuals to these drugs unnecessarily.
Without going into further detail we can see a certain picture forming here; essentially that Catecholamines may play a role in the presentation of ADHD. Considering the working model in regards to a hypercatecholaminergic response post-vaccination, we may raise specific questions as to what role ADHD may play with respect to vaccination.
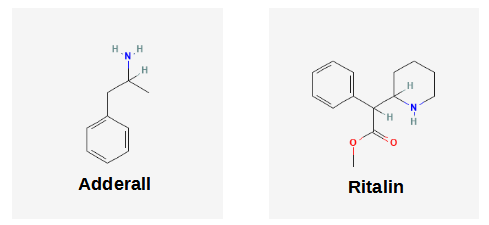
And we may find more evidence when looking at the treatment options for ADHD. Most medications for ADHD are stimulants in the form of Amphetamines (eg. Adderall) or Methylphenidate (eg. Ritalin) and are called sympathomimetic drugs because they mimic endogenous agonists of the sympathetic nervous system. Both drugs work by blocking the reuptake of Dopamine and Norepinephrine, and the elevated levels within the synapse between neurons is what likely attenuates symptoms of ADHD in specific individuals. These stimulants are also known to inhibit the enzyme monoamine oxidase which metabolizes these Catecholamines, which may extend the half-life of these molecules:
The stimulants interact with and inhibit DAT-1 and norepinephrine transporter (NET), thereby inhibiting the reuptake of DA and NE. However, amphetamine also gains access into the presynaptic terminal via DAT-1 and NET to release the stored NTs.51-53 Both stimulants inhibit monoamine oxidase, the enzyme that metabolizes these catecholamines; however, amphetamine is the more potent of the two.14 Thus, the net effect with either stimulant is to rectify the level of NTs such as DA and NE in the synapse. The slightly different mechanism of action between methylphenidate and amphetamine explains why some patients failing to respond to one stimulant show a better response with the other.
Maintaining elevated levels of Catecholamines may help alleviate some of the symptoms of ADHD, but like with many drugs the effects of such Catecholamine reuptake inhibition don’t affect just the brain or nervous system. This effect can also extend to other parts of the body- most notably the cardiovascular system.
Controversy has erupted around ADHD and possible associations to cardiomyopathy, strokes, arrhythmias, and sudden cardiac death (SCD) in those prescribed stimulants.
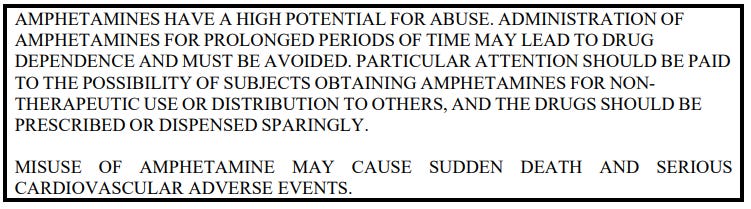
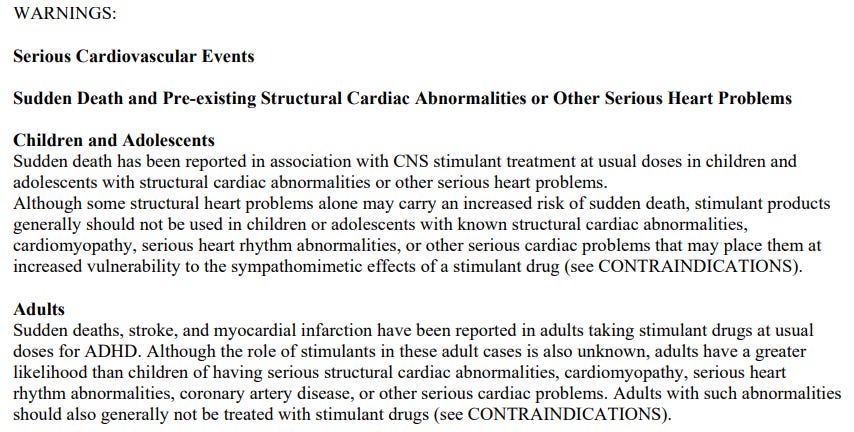
This has led these drugs to carry a “black-box” warning, essentially a warning description with a black border used by the FDA to indicate drugs that carry the possibility of causing serious adverse reactions.
Here’s one black-box warning for Adderall (with more information on Adderall here):
With Adderall the warning section provides this information about risk of cardiovascular disease in both children and adults, which can be severe under certain circumstances:
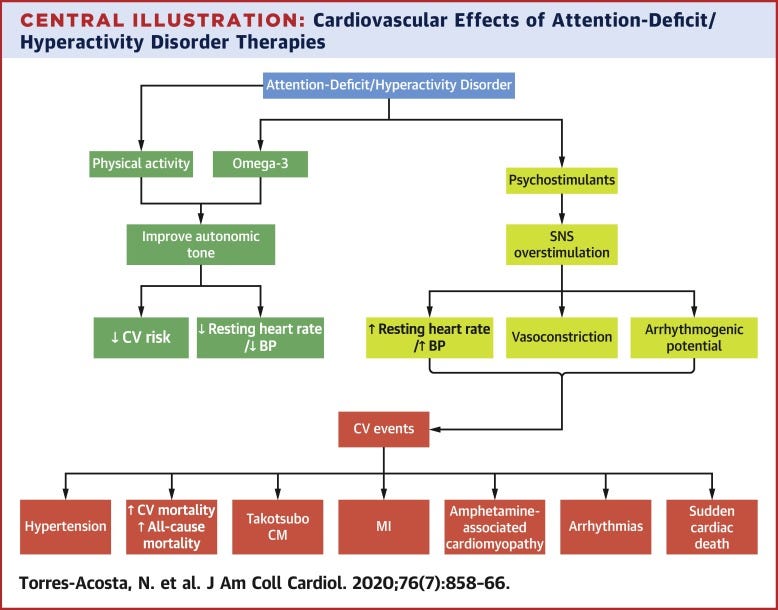
And an outline from Torres-Acosta, et. al.3 provides a good flow of the downstream effects of stimulant use for ADHD. It’s a rather interesting article that contains a succinct examination of the literature while also providing alternatives that should be looked into before considering stimulants4.
In the case of children it’s remarked that contraindicators such as underlying, pre-existing cardiovascular disease may be the culprit in children and adolescents, as the addition of a stimulant may exacerbate these problems leading to the presentation of serious cardiovascular complications and possible death.
With adults, the contraindications are rather muddied (in some regards moreso than children) as some have argued that adults are more prone to cardiovascular disease due to age and lifestyle choices altering heart function (i.e. years of poor eating, lack of exercise, wear on the heart, etc.). However, adults are also more likely to have been prescribed stimulants long-term, and years of amphetamine use may be a causative factor rather than a contraindicator for cardiovascular disease.
It’s worth noting that, in general, these warnings have been considered highly controversial. Several meta-analyses show no increased risk of cardiovascular disease while others suggest that use of stimulants may increase blood pressure and heart rate post stimulant administration5,6- all signs of an elevated Catecholamine response.
Remember that meta-analyses are heavily dependent on the studies sampled and therefore suffer from heterogeneity i.e. differences in sample sizes, demographic differences, underlying comorbidities, medication history, study methodology, biometrics measured, etc. etc.
In regards to sudden cardiac death and ADHD medication use Torres-Acosta, et. al. provides this assessment of the limited number of studies within the literature and indicates some rather concerning findings:
Over the past 3 decades, sporadic cases of SCD have been reported among children using methylphenidate or amphetamines for ADHD (33,34). A matched case-control study of individuals 7 to 19 years of age found an increased risk of SCD in the group taking sympathomimetic stimulants (35). To eliminate the uncertainty related to recall bias, a subgroup analysis of this study was performed based solely on cases with autopsy, toxicology, and medical examiner reports; analysis still showed a positive association between ADHD medications and SCD (35).
Taken altogether, the literature in regards to ADHD, stimulant use, and cardiovascular disease is mired with conflicting evidence.
However, given the fact that ADHD may be a disease of Catecholamine dysfunction, and that the use of stimulants continues to bring with it controversies over CVD and elevated Catecholamine circulation warrants questions as to whether these factors may play a contributing factor in vaccine-induced hypercatecholamineric responses.
In essence, could there be a possible synergistic, hypercatecholaminergic response in association between ADHD, stimulant use, and vaccination?
Now, I need to make this very clear because such a speculation may lead people to take this and run with it to shout how ADHD medications are causing the myocarditis along with the vaccines and shaking their fists at Big Pharma. I am absolutely NOT stating that these ideas should warrant some halting or stopping of ADHD medications. Absolutely DO NOT use this information as medical advice for yourself or loved ones! I wish this goes without needing to be said but considering how many people have taken tenuous associations and have blown them up/exaggerated them I want to be very careful with these assumptions!
Rather, I am making a case that an examination of a hypercatecholaminergic state should look at ALL possible factors, and in which case there may be some evidence that warrants an examination of whether ADHD and the use of stimulants may be a contraindicator for vaccine-induced myocarditis. Combined with the fact that young men are more likely to be diagnosed with ADHD, the fact that stimulants are the go-to, first-line medication to treat ADHD, AND that prescriptions for ADHD have been on the rise the past few years it may be worth investigating whether there may be associations between these factors working synergistically to cause the presentation of myocarditis and SCD in young men.
As to Teenager A from the autopsy report, there is no way of figuring out what exactly happened with his specific case. The coroners note that he stopped taking Amphetamines but make no note as to when he stopped taking them or for how long he was prescribed them.
Given the overwhelming lack of context there’s no way to conclude that ADHD or amphetamines may have played a role in this teenager. However, as the search for answers continue it may be within the interest of researchers and medical professional to investigate if there may be any association between those prescribed amphetamines and possible synergistic responses to vaccines and elevated levels of Catecholamines. Again, it’s the collection of insults that may be worth looking into.
Teenager B: the possible association between obesity and Catecholamines
At this point you may have figured out how I’m organizing my research. Essentially, given the autopsy report and handful of case reports are there any factors that stand out and may provide a lead for further investigation.
For Teenager A the evidence of him having ADHD meant looking into any association between ADHD and Catecholamines. For Teenager B the BMI suggests that he was obese, and that provides a possible lead into searching for any evidence relating obesity and Catecholamines.
From the autopsy report:
Boy B had no complaints, prior health issues, or prior SARS-CoV-2 infection. Neither boy complained of fever, chest pain, palpitations, or dyspnea. The autopsies were unremarkable except for obesity in one boy [Boy B] and the cardiac findings […]
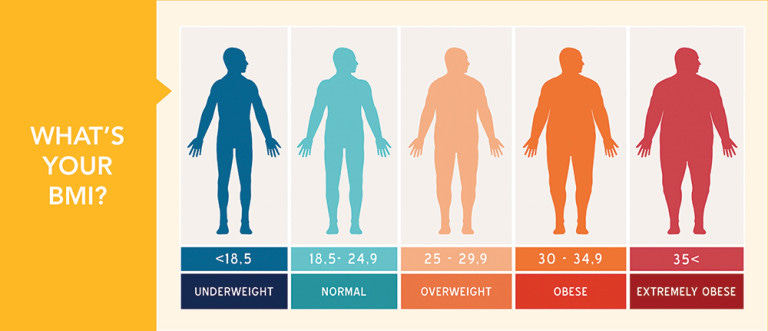
BMI is short for body-mass index, and it’s a measure that takes into account one’s weight and proportions to provide a numerical value7. Higher BMI values generally correlate with comorbidities such as high blood pressure, diabetes, cardiovascular disease, cancer risk, and a weakened immune system.
A normal BMI range is one between 18.5-24. Increments of 5 that go above 24 enter into territories of overweight, then obese, then morbidly obese, and so on.
Rates of childhood obesity have been on the rise since the past few years, with some measures from the CDC indicating a childhood obesity prevalence of up to 20%:
And a study published in the Journal of the American Medical Association (JAMA) last year also corroborated evidence of weight gain among children during lockdowns, providing further evidence that the lockdowns have had a detrimental effect on the young.8
Similar to ADHD the prevalence of obesity shows a disproportionately higher rate among boys compared to girls as indicated in this BMJ article9:
The difference in prevalence of obesity for boys and girls has also been reported previously. For example, National Canadian data (2004–2013) consistently observed a higher prevalence of obesity in boys compared with girls aged 3–19.4 A two-fold higher prevalence of severe obesity in boys compared with girls aged 5–9 has also been observed in Canada.5 Similarly, in China, the prevalence of childhood obesity steadily increased over a 25-year period (1985–2010) and was consistently higher among boys than girls aged 7–18.6 From 2000 to 2010 in Poland, the prevalence of both overweight and obesity in children aged 3–19 increased, with a greater prevalence in boys than girls.7
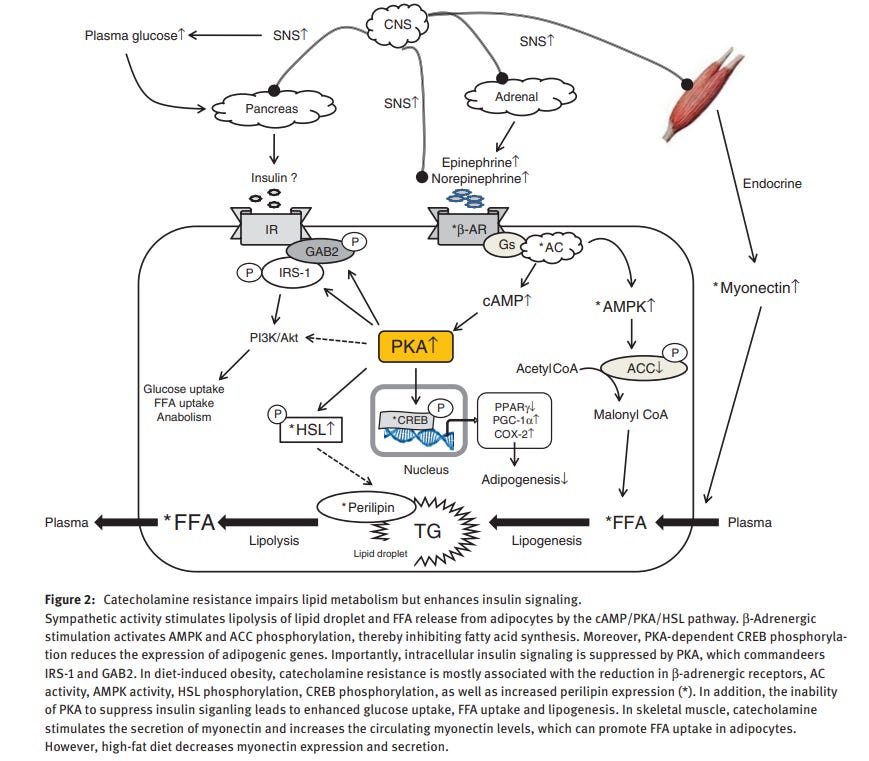
As to the mechanism of action, Catecholamines appear to have an effect on lipolysis (breakdown of fat; antithesis of lipogenesis which is formation of fat), and it’s suggested that this relationship is what influences obesity and provides a possible link between Catecholamines and weight gain (Zouhal, et. al.10):
Catecholamines are known to stimulate lipolysis via the b1- and b2-adrenoceptors, which enhance the intracellular cyclic adenosine monophosphate (cAMP) concentration via cAMP-dependent protein kinase activation, leading to the phosphorylation and activation of hormone-sensitive lipase (HSL) [5]. Inversely, stimulation of a2-adrenoceptors by catecholamines inhibits lipolysis [5]. These adrenergic responses depend on the density of these two families of receptors, their relative affinities, and the location and amount of adipose tissue [6, 7]. Obesity may modify a- and b-adrenoceptor sensitivity in adipose tissue and thus the effect of catecholamines on the lipolytic process, increasing adipose fat storage [8, 9]. Some authors even suggest that the altered activity of the SNS is the main cause of obesity [10].
So we can see here that lipolysis may be a consequence of the adrenergic receptor type (alpha or beta) that is being stimulated, which makes elucidating the actual role of Catecholamines rather difficult.
This association is made even more confusing as obese individuals tend to show reduced levels of circulating Catecholamines:
While obese subjects often display an increased basal SNS activity, there are numerous reports of blunted adrenal medulla function (reduced epinephrine secretion) in this population [16–18] (epinephrine: 6.20; 6.04 and 5.51 lg/24 h for BMI \25.0; 25.0–27.6 and [27.6 kg/m [2], respectively). The lower catecholamine response observed in the obese population seemed to be affected by high plasma levels of circulating leptin [75], insulin [76] and cortisol [18]. These hormones could exert an inhibitory effect on catecholamine production. Also, a higher catecholamine elimination rate may be responsible for the lower plasma catecholamines in obese populations.
There’s also a matter of whether altered Catecholamine responses are attributed to the eventual increase in body weight and obesity, or if obesity is the reason for the altered response to Catecholamines.
So although obese individuals tend to show reduced levels of circulating Catecholamines, it could be the alterations in adrenergic receptor sensitivity to Catecholamines that is important within the context of obesity.11
A review from Lambert, et. al.12 provides some context to the uneven data, citing that measures of Catecholamines may differ between studies and may alter interpretations of said studies:
Early work and opinion by Bray [3] provided the impetus for studying sympathetic nervous function in obesity with the idea that diminished basal SNS activity, in not providing the normal calorie-wasting thermogenic response to overeating, may cause positive energy balance and possibly contribute to the development of obesity. However, initial studies in humans lead to a high level of disagreement concerning the state of SNS function in obesity. In their thorough review of the literature, Young and McDonald [32] reported that there was a similar number of studies reporting that SNS was low, normal or elevated in human obesity. The reliance of these early studies on venous and urinary noradrenaline concentrations, which at best provides an imprecise measure of sympathetic tone, perhaps contributed to the heterogeneity of the data, as may the fact that regional sympathetic outflow to the organs is not uniform. Indeed, using measures of regional noradrenaline isotope dilution Mario Vaz and colleagues [29] clearly demonstrated variations in sympathetic tone among vascular beds in human obesity, with SNS activation being evident in the kidneys, but absent in the heart.
So what exactly is going on in obesity and Catecholamines? If we look at elevated levels of blood pressure and heart rate one may consider that these are indicative of some association with Catecholamines. Considering that obesity can eventually lead to CVD there may be some considerations in favor of long-term responses to Catecholamines. But these arguments are merely observational, and for adults the general opinion appears to be that sympathetic nerve response to Catecholamines are attenuated due to reduced Catecholamine levels.
As to childhood obesity, there’s been contrasting evidence that suggests that an actual sympathetic overdrive may be related to childhood obesity. Rather than reduced levels of Catecholamines, it may be an overactive level that leads to eventual Catecholamine resistance (reduced sensitivity to Catecholamines) that may be responsible (Qi, Z. & Ding, S.13):
Sympathetic overactivity occurs in obese animals, as evidenced by increased blood pressure, cardiac output, heart rate as well as the activation of renin-angiotensinaldosterone system (6). Obesity-related hypertension in pediatric patients is a consequence of the childhood obesity with the activation of the renin-angiotensinaldosterone system (RAAS) and the stimulation of sympathetic nervous system (7). Significantly, adipose tissue lipolysis shows a decreased sensitivity to epinephrine in childhood obesity. This resistance to catecholamines occurs during the dynamic phase of fat accumulation, suggesting that epinephrine resistance might be the cause rather than the result of childhood obesity (8, 9).
This hypothesis from Qi, Z. & Ding, S. proposes that Catecholamines are intrinsically linked to insulin and leptin, and that Catecholamine resistance may not be able to dampen insulin signaling and may be an actually driver for childhood obesity. Essentially, as cellular responses to Catecholamines dampen insulin levels may go unchecked, and it could be these elevated levels of insulin that drive weight gain and obesity.
The hypothesis is constructed below:
Further, we propose that childhood obesity should not be caused by insulin resistance, but by the inability of catecholamine to inhibit insulin action. In contrast to the current dogma, it is elevated insulin signaling in the fat that leads to lipogenesis and childhood obesity. High-fat diet and stress induce chronic SNS activation. As a result, the catecholamine resistance promotes the progression of lipid accumulation at the upstream of insulin signaling (Figure 2).
There’s a few questions as to the veracity of such a hypothesis as it proposes a possible role reversal in children compared to adults, such that the overactive sympathetic response in children leads to eventual Catecholamine resistance whereas in adults Catecholamine production may decline due to obesity and actually lead to reduced sympathetic activity. However this argument would need to take into account the increased risk of cardiovascular disease in both demographics and the influence of Catecholamines on the heart.
If all of this sounds rather confusing, it is! Much of the evidence for obesity and associations to Catecholamine release is rather limited and highly contextual, so extrapolating research from these papers can cause a lot of confusion.
Obesity itself is known to come with a host of issues, including more severe illness from COVID and poor responses to vaccines. It’s the latter that may complicate the matters even further.
In short, the actual biochemical pathways responsible for Catecholamine and its association to obesity is difficult to discern, but as proposed by the Qi, Z. & Ding, S. hypothesis there may be some consideration for a hyperactive sympathetic system as being a precursor for obesity and may point to elevated Catecholamine levels.
Just to make this even more difficult (because why not!), there have been studies looking at links between obesity and ADHD, with some suggesting that there may be some association14,15, although this may be a consequence of behavior rather than biochemical relationships between the two (i.e. Catecholamines affecting ADHD and Obesity).
For Teenager B the situation is even worse compared to Teenager A . There’s really no way of extrapolating from the limited patient information to figure out what effects the obesity may have had on his health prior to the introduction of the mRNA vaccines, or if there would be any indication of possible hypercatecholaminergic situations beforehand that may have been cause for concern. The obesity is rather alarming in a teenager, but compared to the possible associations between ADHD, stimulant use and Catecholamines there isn’t much to work with here. Nonetheless, the information does provide another possible factor that may be worth considering in the grand scheme of synergistic myocarditis.
Given how long this post has gotten I will save my review and pontifications on athletes for the next post. For now, the limited information provided with the two teen males provided avenues to go down. Although the overall evidence is rather conflicting, and in the case of obesity highly confusing, it reminds us that multiple factors are at play that add onto our overall health. When examining what specifically is causing the myocarditis and SCD seen post-vaccination we should take care not to look at vaccines alone and exclude other features that may work together with the vaccines to cause the serious adverse reactions being seen.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

James R. Gill, Randy Tashjian, Emily Duncanson; Autopsy Histopathologic Cardiac Findings in 2 Adolescents Following the Second COVID-19 Vaccine Dose. Arch Pathol Lab Med 1 August 2022; 146 (8): 925–929. doi: https://doi.org/10.5858/arpa.2021-0435-SA
Sharma, A., & Couture, J. (2014). A review of the pathophysiology, etiology, and treatment of attention-deficit hyperactivity disorder (ADHD). The Annals of pharmacotherapy, 48(2), 209–225. https://doi.org/10.1177/1060028013510699
Torres-Acosta, N., O'Keefe, J. H., O'Keefe, C. L., & Lavie, C. J. (2020). Cardiovascular Effects of ADHD Therapies: JACC Review Topic of the Week. Journal of the American College of Cardiology, 76(7), 858–866. https://doi.org/10.1016/j.jacc.2020.05.081
Don’t take these alternatives as an indication to stop ADHD medications! Remember to always consult a medical professional on advice!
Hennissen, L., Bakker, M. J., Banaschewski, T., Carucci, S., Coghill, D., Danckaerts, M., Dittmann, R. W., Hollis, C., Kovshoff, H., McCarthy, S., Nagy, P., Sonuga-Barke, E., Wong, I. C., Zuddas, A., Rosenthal, E., Buitelaar, J. K., & ADDUCE consortium (2017). Cardiovascular Effects of Stimulant and Non-Stimulant Medication for Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis of Trials of Methylphenidate, Amphetamines and Atomoxetine. CNS drugs, 31(3), 199–215. https://doi.org/10.1007/s40263-017-0410-7
Liang, E. F., Lim, S. Z., Tam, W. W., Ho, C. S., Zhang, M. W., McIntyre, R. S., & Ho, R. C. (2018). The Effect of Methylphenidate and Atomoxetine on Heart Rate and Systolic Blood Pressure in Young People and Adults with Attention-Deficit Hyperactivity Disorder (ADHD): Systematic Review, Meta-Analysis, and Meta-Regression. International journal of environmental research and public health, 15(8), 1789. https://doi.org/10.3390/ijerph15081789
To figure out your own BMI you can find calculators all over online. Here’s a link to one for those interested:
https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
Woolford SJ, Sidell M, Li X, et al. Changes in Body Mass Index Among Children and Adolescents During the COVID-19 Pandemic. JAMA. 2021;326(14):1434–1436. doi:10.1001/jama.2021.15036
Shah B, Tombeau Cost K, Fuller A, et al
Sex and gender differences in childhood obesity: contributing to the research agenda
BMJ Nutrition, Prevention & Health 2020;3:doi: 10.1136/bmjnph-2020-000074
Zouhal, H., Lemoine-Morel, S., Mathieu, M. E., Casazza, G. A., & Jabbour, G. (2013). Catecholamines and obesity: effects of exercise and training. Sports medicine (Auckland, N.Z.), 43(7), 591–600. https://doi.org/10.1007/s40279-013-0039-8
There’s some indication that alpha receptor responses to Catecholamines are altered in obese individuals, as seen in the review:
Subcutaneous abdominal adipocytes of obese individuals show a higher a2-adrenergic response to catecholamines than subcutaneous abdominal adipose cells from lean subjects [11]. Also, according to De Glisezinski et al. [12], obese subjects at rest present decreased b-adrenergic stimulation of lipolysis. More recently, a study by Jocken et al. [56] showed in vivo that obese participants have a blunted b-adrenergically mediated lipolytic response per unit of adipose tissue. The a2-adrenergic component of subcutaneous abdominal fat cells has also been shown to be directly proportional to the level of total body fat in men [11].
Lambert, E. A., Straznicky, N. E., & Lambert, G. W. (2013). A sympathetic view of human obesity. Clinical autonomic research : official journal of the Clinical Autonomic Research Society, 23(1), 9–14. https://doi.org/10.1007/s10286-012-0169-3
I will say I’m rather partial to a punny title.
Qi, Z., & Ding, S. (2016). Obesity-associated sympathetic overactivity in children and adolescents: the role of catecholamine resistance in lipid metabolism. Journal of pediatric endocrinology & metabolism : JPEM, 29(2), 113–125. https://doi.org/10.1515/jpem-2015-0182
Kummer, A., Barbosa, I. G., Rodrigues, D. H., Rocha, N. P., Rafael, M., Pfeilsticker, L., Silva, A. C., & Teixeira, A. L. (2016). Frequência de sobrepeso e obesidade em crianças e adolescentes com autismo e transtorno do déficit de atenção/hiperatividade [Frequency of overweight and obesity in children and adolescents with autism and attention deficit/hyperactivity disorder]. Revista paulista de pediatria : orgao oficial da Sociedade de Pediatria de Sao Paulo, 34(1), 71–77. https://doi.org/10.1016/j.rpped.2015.06.013
Cortese, S., & Tessari, L. (2017). Attention-Deficit/Hyperactivity Disorder (ADHD) and Obesity: Update 2016. Current psychiatry reports, 19(1), 4. https://doi.org/10.1007/s11920-017-0754-1




I am honored beyond words. Kind of you to mention me, and I really did enjoy reading your careful exegesis … as always, I also get an awful lot from the discussions that ensue. Susan’s intelligent point below, for example.
My first issue with the vaccine rollout was that there was no requirement for a person to get medical clearance from their doctor to receive the vaccine. This was especially disconcerting to me because the first people authorized to receive the vaccine were people with pre-existing morbidity conditions. This would mean they were already on at least 1 type of medication long term and possibly several. I believed there should have at least been a consultation required with their doctor to determine possible drug-interactions. Alas silly me.. how could there be a way to determine possible drug interactions with the ingredients in the vaccine are not fully known... still to this day.
Yes, the medications given for ADHD have the potential side effect for risk of cardiovascular damage. Since there are so many children on this medication from a very early age... this SHOULD HAVE BEEN A BLACK BOX WARNING FOR THEM given by the FDA for all vaccines.
FOR SHAME....