New research provides insight into Adenoviral-based COVID vaccine blood clots
With a mechanism that is so obvious why exactly did it take 3 years to figure out?
When it comes to COVID vaccine adverse events there has been much speculation but not much clear, concrete evidence. It doesn’t help that those within the medical establishment have failed to do their due diligence in researching why some people are experiencing the multitude of adverse events being reported, and this has led many people to have to formulate their own hypotheses.
With respect to the adenoviral-based vaccines in particular, there is even less research directed towards finding out why people experience relatively high rates of a phenomenon called vaccine-induced immune thrombocytopenia and thrombosis (or VITT) compared to other vaccines. And now that most of these vaccines have been removed from market research incentive has also likely halted for the most part.
The only prevailing hypotheses i.e. the only hypothesis that has been entertained has suggested that pockets of high negative charges on parts of the adenoviral surface may bind to the highly positive cytokine Platelet Factor 4 (PF4). This binding appears to allow for a change in the presentation of PF4 that makes it immunogenic and allows for binding of anti-PF4 antibodies. Continuous formation of adenovirus vaccine/PF4 complexes allow for more anti-PF4 antibodies to bind and thus leads to the paradoxical cascade of clotting sans any platelet formation.
This has been highlighted in a prior post:
Adenoviral Vector Redux
Modern Discontent is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.Thank you for reading Modern Discontent. This post is public…
The work was made more evident by the fact that both those who experienced VITT and those who take blood thinners such as heparin both appear to present with anti-PF4 antibodies, and in fact it’s the correlation between heparin-induced thrombocytopenia and the initial presentations of VITT that helped to form this prevailing hypothesis.
Unfortunately, the trail for further research into this mechanism went cold, much to the chagrin of those who experience VITT and those who are trying to seek out answers.
Now, for anyone with a sense of intuition, and hopefully something I highlighted previously, one would see such a hypothesis and believe that the best course of research would be to look into adenoviruses and see whether infections themselves are known to produce anti-PF4 antibodies. Obviously, if such an event were present in the literature then we would have a trail that could provide further insights into drawing a direct relationship between the adenoviral vector itself and the cause of VITT.
Unfortunately, I couldn’t find anything regarding anti-PF4 antibodies and adenoviral infections, meaning that there has been a huge gap in the literature even though this would be an avenue worth researching. And even with the first instances of VITT there is no clear endeavors to look into this association. Again, it seems like it would be an obvious thing to look into given that VITT are somehow more prevalent among adenoviral-vaccine recipients and it is one of the main differences in vaccine formulation relative to the other things on the market.
And yet it would take just until last week for a very small editorial to suggest this exact thing- that anti-PF4 antibodies produced by those with VITT share remarkable similarity to people who experience anti-PF4 antibodies following an adenoviral infection.1

Again, this work is very small and focuses on very few participants. Nonetheless, the researchers took to looking into something that not many people have looked into.
That is, what antibodies are people producing that are anti-PF4 antibodies?
For a while we have discussed how critical antibodies are to fighting off infections. Although the entirety of the immune system should be evaluated antibodies do work as one critical component of our adaptive immune system.
However, what many people may not know is that the antibodies we produce aren’t all similar to one another. That is, even though two people may produce antibodies to help fight against SARS-COV2 it doesn’t mean that these same two people are producing the same antibodies as one another.
This has been overlooked quite often in immunology research, and funnily enough something that I have mentioned before as an issue with discussions on immunology since the type of antibodies (or really the sequence on the heavy and light chains) people produce are likely to greatly vary from person to person.
Thus, it’s not the number of antibodies but the type of antibodies that provide better context.
Here, the researchers took to examining the antibody makeup of a few people who have VITT, and noted that all of the participants carried the same allele for a heavy-arm chain sequence:
All the patients with VITT who have been evaluated have expression of the IGLV3-21*02 allele and a heavy-chain motif, resulting in at least eight acidic (negatively charged) amino acids of the paratope (antigen-binding region), by which anti-PF4 antibodies bind to their antigen. These negatively charged regions mediate strong binding of the antibodies to the positively charged arginine and lysine residues on PF4.5
Remember that PF4 is argued to be highly positive, and this explains why PF4 may bind to both heparin and highly negative regions on the adenovirus vector. Therefore, it wouldn’t be surprising that an antibody bearing a highly negatively-charged paratope would also bind with PF4 well- this is a clear case of opposites attracting.
Here, the negatively charged amino acid sequences are shown in red, which also includes a mutation in one portion of the light-chain from a positively charged lysine into negatively charged glutamate and aspartate:
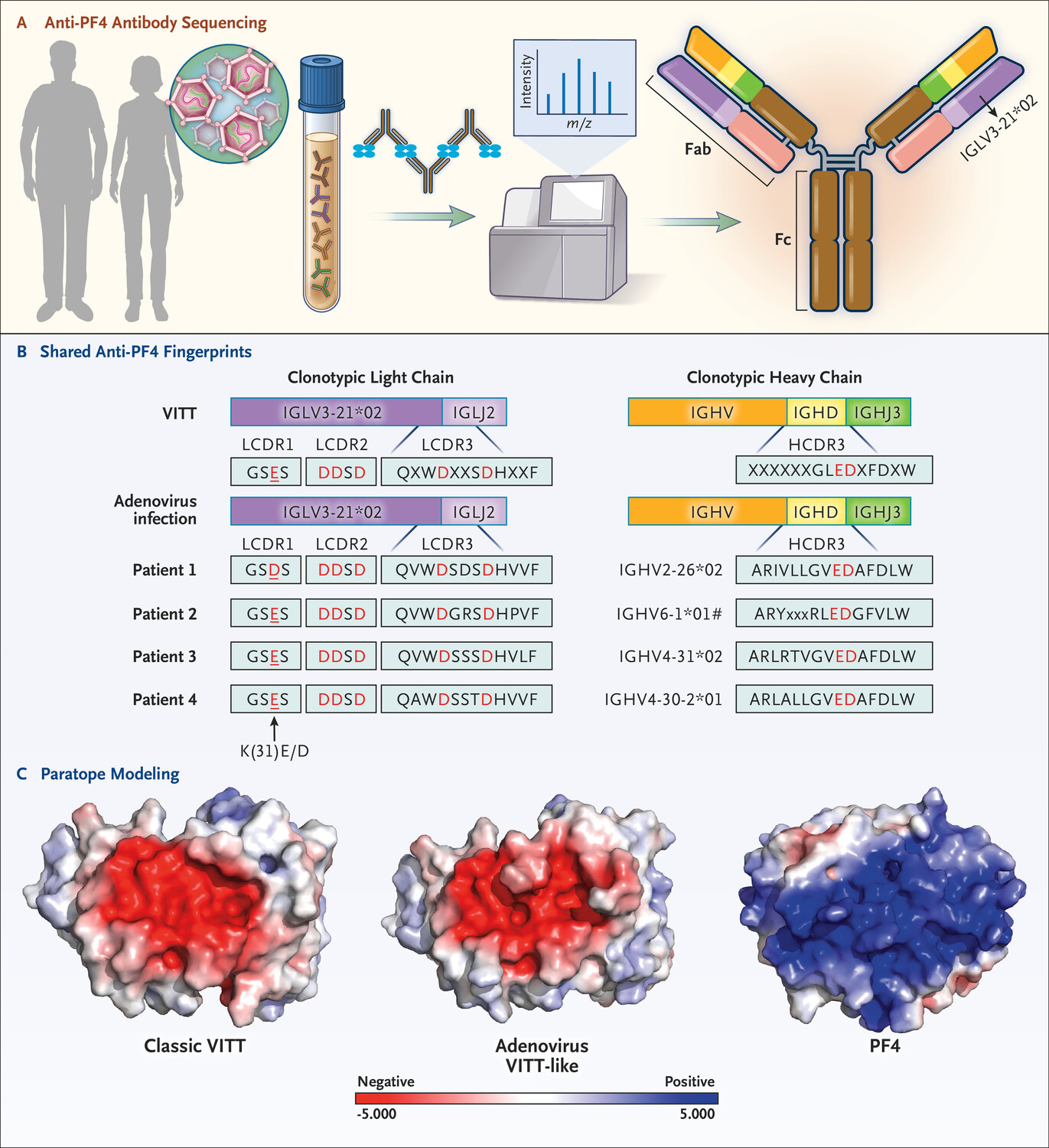
In Figure 1B a representative sequence of someone with VITT is shown at the top. The sequence of 4 people who were previously infected with an adenovirus and positive for anti-PF4 antibodies are shown below that sequence.2 In all those instances note that the amino acid in those 8 positions are homologous, suggesting that the antibodies produced in response to adenoviral-based vaccines and to adenoviral infections themselves may be the same.
The authors put these findings in the following way:
We conclude that the antibodies induced by adenoviral vector–based Covid-19 vaccination (classic VITT) and the VITT-like antibodies induced by natural adenovirus infection are extremely similar. Such an extraordinary level of autoantibody fingerprint identity between two disorders — at the level of patient-derived antibodies — strongly indicates that VITT and the anti-PF4 disorder that is associated with adenoviral infection are a distinct class of adverse immune responses associated with viral (presumably, adenoviral) structures.
Our findings indicate that the anti-PF4 disorder that was first recognized as VITT is essentially identical to the disorder caused by adenovirus infection that occurs sporadically. Thus, the clinical lessons learned from VITT remain relevant: thrombosis associated with thrombocytopenia with greatly elevated d-dimer levels — particularly after a viral infection — may be investigated and treated as an anti-PF4 disorder.
Be aware that this work is rather preliminary- more participants and greater assessment of both VITT patients as well as patients who experience anti-PF4 antibodies post-adenovirus infection is needed to better establish this link.
Nonetheless, this is the closest that we have gotten to finding an actual causal link between VITT and the vaccines, and the answer lied in none other than examining those who were infected with adenoviruses- the exact place where people should look in order to make proper comparisons!
So although this editorial provides additional insights into VITT it’s also frustrating that it took this long to do something that should have been so obvious to any researcher! How many people thought to look into those who had adenoviral infections to see if they produced anti-PF4 antibodies? Why is the literature scant with this possible autoimmune disease? And how many blood clotting disorders have gone unrecognized for possibly being anti-PF4 in nature and stemming from viral infections?
All of this highlights obvious pitfalls in research where something that should be rather easy to intuit took so long to finally be researched. It probably helps to explain why research is in such a sad state as it is when things that should seem obvious don’t appear obvious to many people.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists such as myself to provide work outside of the mainstream narrative.

Wang, J. J., Schönborn, L., Warkentin, T. E., Chataway, T., Grosse, L., Simioni, P., Moll, S., Greinacher, A., & Gordon, T. P. (2024). Antibody Fingerprints Linking Adenoviral Anti-PF4 Disorders. The New England journal of medicine, 390(19), 1827–1829. https://doi.org/10.1056/NEJMc2402592



Yet another reason why blanket mandates that every single person get vaccinated were insane. If individual responses are genetically based and can vary so widely, there's no way to know how individuals will react. I hope that in the future we'll figure out some way to get care tailored to each person's genetic makeup.
Self centered researchers, can only look in their very tiny microscopes... no awareness of anything outside of that... or its consequences.
Are there any adeno vaxes still being given?