Following along with the prior post on minerals this post will focus on vitamins. In particular, we will take a look at vitamin C and D and see whether these vitamins may help with managing hypertension.
Similar to prior posts remember that the information presented in this article is intended to be informative, not prescriptive.
II. Vitamins & Hypertension
Given that vitamins have broad effects on the body it should come as no surprise that vitamins may help to control hypertension.
In general, studies relating vitamin supplementation to reduced hypertension have presented with varied results, mostly owed to differences in dosing and groups tested.
What’s interesting is that there appears to be a discrepancy between hypertensive individuals and normotensive individuals when it comes to the effects of vitamins, suggesting that correction of physiological impairments or nutrient deficiencies may be critical outcomes.
As not all vitamins can be looked at, the current article will look solely at vitamin D and C in particular.
a. Vitamin C Deficiency & Hypertension
Vitamin C, also known as ascorbic acid, is a water-soluble, essential vitamin found in many fruits and vegetables.
Vitamin C is critical for many bodily functions by serving as a precursor for critical compounds, however many of its actions are derived from its ability to act as an antioxidant.
As it relates to vascular disease it’s been suggested that vitamin C helps to activate the expression of nitric oxide synthase, an enzyme responsible for production of nitric oxide- a key signaling molecule in relaxing endothelium (this will be covered in more detail in another post). It’s also been suggested that the antioxidative effect of vitamin C may reduce cellular oxidative stress and thus reduce damage to blood vessels as well, which may also aid in endothelial function.
A review from May, J. M., & Harrison, F. E1 elaborates on the relationship between vitamin C and its antioxidant effects on endothelium:
Ascorbate has long been considered a key cellular antioxidant, serving as a primary antioxidant by detoxifying exogenous radical species that have entered cells or which have arisen within cells due to excess superoxide generation by mitochondrial metabolism, by NADPH oxidase, xanthine oxidase, or by uncoupled nitric oxide synthase (NOS). As previously noted, at the low millimolar concentrations of ascorbate likely to exist in endothelial cells, ascorbic acid will aid superoxide dismutase in scavenging superoxide and its more toxic breakdown products (Fig. 3). The question arises as to just how much intracellular ascorbate contributes to the antioxidant capacity of cells.
Endothelial cells may utilize vitamin C to repair oxidized lipids and proteins, appearing to undergo a recycling mechanism with the cofactor Tetrahydrobiopterin (BH4), a molecule utilized by nitric oxide synthases that also helps to sustain nitric oxide levels:
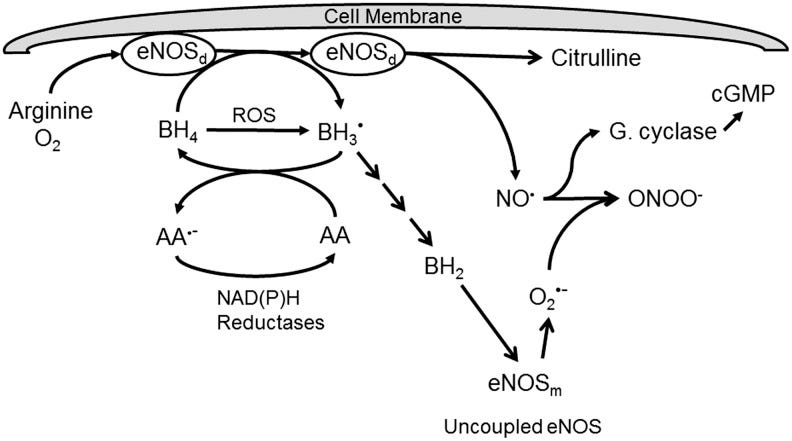
So it appears that much of vitamin C’s antihypertensive mechanisms may relate to its antioxidant effects, with one prevailing hypothesis linking vitamin C to maintaining nitric oxide levels.
When it comes to the actual effects of vitamin C supplementation on reducing blood pressure results have been highly varied.
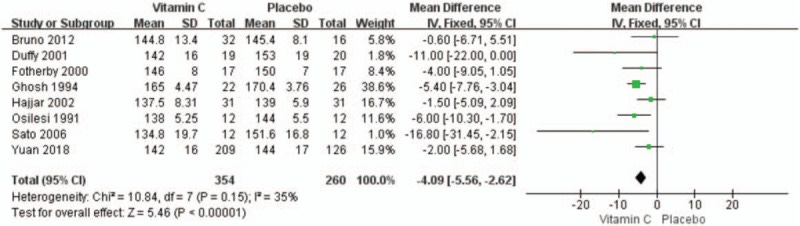
In one systematic review/meta-analysis from Guan, et al. 2 8 RCT’s were examined for vitamin C's effects on systolic and diastolic blood pressure (SBP and DBP, respectively), noting that the given studies appeared to show a benefit in supplementation with vitamin C. Only SBP is shown below, although the results seemed comparable for DBP as well.
The participants included in these 8 RCT’s apparently had essential hypertension, leaned older with mean ages ranging from 46-78 between studies, and had a range of vitamin C supplementation ranging from 300-1000 mg/dL. For SBP the weighted mean difference in the studies provided showed a 4.09 mmHg reduction in SBP for the vitamin C group compared to controls3.
Several studies haven’t appeared to show a benefit in vitamin C supplementation, likely due to differences in study design such as small sample size, age of participants, hypertensive status of participants, as well as dosing levels and duration.
It appears that the effects are more pronounced in hypertensive and older patients while normotensive patients don’t seem to have the same level of benefits. This may indicate that hypertension may be associated with lower vitamin absorption as well as physiological dysfunction as one gets older. In such cases supplementation may help to reduce deficiencies and help to partially attenuate high blood pressure that may come about due to such age-related factors.
However, note that vitamin C deficiency is very rare with cases of scurvy4 (daily vitamin C intake below 10 mg/day that persists for several weeks) being very uncommon in developed nations and may only occur in those with very limited food sources. Therefore, a majority of people are likely to have adequate vitamin C levels which may explain a mechanism of hypertension unrelated to vitamin C.
So overall, the evidence towards vitamin C use in helping hypertension is conflicting. More research would be needed to see the true scope of vitamin C’s benefit, although it’s also worth noting that vitamin C has a high dosage upper limit of around 2,000 mg/day, which may be difficult to reach unless overusing supplements, so the risk of toxicity is generally low.
Nonetheless, more diverse food sources would do more than to just provide vitamin C and thus may be good for overall health. Food sources rich in vitamin C include fruits such as citrus and strawberries, dark and/or leafy greens such as kale, spinach, and cruciferous vegetables such as brussels sprouts and broccoli, as well as different varieties of peppers.
Additional readings on vitamin C and heart health can be found below. Note that these articles aren’t specific to hypertension.
Moser, M. A., & Chun, O. K.5: Vitamin C and Heart Health: A Review Based on Findings from Epidemiologic Studies
This review includes a meta-analysis that suggests a beneficial effect of vitamin C on both systolic and diastolic blood pressure. The meta-analysis included 29 different studies with a mean vitamin C supplementation level of 500 mg/day.
Morelli, et al.6: Vitamin C and Cardiovascular Disease: A Review
b. Vitamin D & Hypertension

Vitamin D is a fat-soluble vitamin that’s grown in significance in recent years. Prior evidence has assumed that vitamin D was only critical for calcium homeostasis. However, more evidence points to many other physiological roles of the vitamin including in immune function, chemical signaling, and hormone regulation, leading some scientists to argue that vitamin D may be looked more as a hormone rather than a vitamin.
More information on vitamin D can be found from a review by Bickle, D.D.7
The discovery of vitamin D came about due to the presence of rickets, a disease of weakened and soft bones in children. The disease gained prevalence during the turn of the Industrial Revolution as smoke-filled urban environments reduced sun exposure and thus conversion of vitamin D.
It was later found that irradiated food provided to children helped treat rickets, and further clinical evidence suggested that exposure of infants to sun and UV radiation were also viable treatments. Both discoveries suggested a mechanism by which some precursor molecule could aid in rickets, with the latter pointing to an in vivo molecule which was later discovered to be vitamin D2 which gets converted to vitamin D3 via UV light.
The conversion into D3 generally takes place in the epidermis with further metabolism via addition of hydroxyl groups (OH) called hydroxylation occurring in the liver and other organs leading to the active metabolites 1,25(OH)2D3 and 24,25(OH)2D3. The numbers indicate where on the original structure hydroxyl groups were added.

Further investigation into vitamin D3’s role in human health would eventually lead to the discovery of vitamin D receptors (VDR) all throughout the body, suggesting a broader, more critical role of vitamin D3 in health.
Not surprisingly, the widespread presence of VDR appears to affect the RAS of many cells and organs.
As outlined in a review from Legarth, et al.8 an in vitro study noted that low vitamin D in juxtaglomerular cells (kidney cells responsible for renin production) led to the activation and production of renin. However, in the presence of the active vitamin D metabolite 1,25(OH)2D3 VDR may form a complex and interfere with the cAMP-PKA pathway that produces renin.

Remember that renin is further metabolized to produce angiotensin and angiotensin II, with the later being a pivotal player in hypertension, and so suppression of renin would have downstream effects in attenuating hypertensive signaling via the RAS.
Many organs and tissues have their own RAS, and as reported by Legarth, et al. vitamin D appears to help regulate the RAS axis of various organs to help improve function and reduce cellular damage. Several animal studies, as well as some cross-sectional studies in humans suggest that the antagonistic effect of vitamin D on RAS may be one factor in alleviating elevated blood pressure. This has led to some research attempting to target vitamin D receptors as a possible method of treating hypertension.9
Interestingly, the link between vitamin D and calcium homeostasis may also play a role in this antihypertensive effect. It’s been suggested that high sodium levels have corresponded with increased intracellular vitamin D and calcium levels. However, as noted in a review from Vaidya, A., & Forman, J. P.10 this dynamic is not well understood as being prohypertensive or antihypertensive:
Resnick and colleagues10,11 speculated that, in the setting of a sustained dietary sodium load, 1,25(OH)2D production and calcium flux into cells were increased, resulting in reduced RAS activity and increased vascular smooth muscle tone. Although this hypothesis bridged the independent implications of sodium, calcium,14–19,22,23,27 and parathyroid hormone28–35 directly in the regulation of the RAS and blood pressure, it did not explain whether the calcium-regulatory role of 1,25(OH)2D on blood pressure was prohypertensive or antihypertensive. Rather, these experiments established a unique interplay among dietary sodium, the RAS, and 1,25(OH)2D on vascular tone that is incompletely understood. Further understanding of these complex relationships may improve the understanding of the role of vitamin D in blood pressure physiology.
The previous post noted that calcium, potassium, and magnesium levels may help to balance out sodium levels, so in some regard vitamin D may also help to provide a regulating factor in circulating mineral levels.
Aside from these effects, vitamin D is considered to improve endothelial function via regulation of NO production, reduction of inflammation of endothelium, as well as a few other mechanisms.
Given the endogenous mechanism of creating vitamin D it would be strange consider that much of the world would be deficient in D, and yet D deficiency is one of the most prominent vitamin deficiencies in the world.
A review from Palacios, C., & Gonzalez, L.11 compiled data from various studies across the globe and displayed the prevalence of vitamin D deficiency among the given countries, noting a high rate of vitamin D deficiency worldwide:

It’s important to remember that the information displayed is contingent upon the studies used and more than likely does not reflect the entire population of given countries. Also, the data collected went up to 2013 (the article published in 2014) so the numbers presented may also be outdated. Samples marked as “Representative Sample” may be more indicative of a population-wide study and therefore may be a better correlator to actual vitamin D status.
Given these global deficiency of vitamin D one may wonder if low vitamin D may be correlated with high prevalence of hypertension.
Several studies have noted a correlation between vitamin D deficiency and increased risk of cardiovascular disease.
However, similar to vitamin C and other clinical studies on supplementation the results for vitamin D have been mixed.
One key issue in many of these studies is the hypertension status of the individual, as well as their vitamin D levels.
A review from Chen, et al.12 which categorized clinical evidence based upon the hypertension and vitamin D status of individuals noted that vitamin D supplementation may benefit those who are both hypertensive and deficient in vitamin D while the effect may not be as robust in hypertensive patients with adequate vitamin D levels.
It’s worth noting that studies that utilized high doses of vitamin D over several weeks were not able to reach adequate vitamin D levels, and so it’s possible that deficiency may still be associated with increased risk of hypertension but that the doses used in clinical studies aren’t able to adequately raise vitamin D levels.
This is noted in the Discussion of Legarth, et al.:
As mentioned in the previous sections, epidemiological studies find some proof of an inverse correlation between serum vitamin D-status and prevalence of EH. However, the overview of interventional studies in Table 3 does not give a clear picture of vitamin D supplementation in relation to cardiovascular health. It is of interest whether vitamin D therapy in the intervention group (vitamin D deficiency at baseline) is able to raise serum 25(OH)D to the optimal levels (30–80 ng/mL) [58]. Common to the three RCTs is that they all show no effects from vitamin D supplementation in 24-h SBP [52,53,54]. These three studies share that the intervention groups at time endpoint are still insufficient in serum 25(OH)D levels. Common to Witham et al. trials is the high-dosage of oral administered cholecalciferol (100,000 IU) given at least two months apart [53,54]. This does not seem to restore the 25(OH)D levels, which can possibly explain the lack of effect on BP. In order to obtain positive effects of vitamin D therapy, there is something that suggests the dose interval to be short (e.g., daily or weekly administration).
So it’s possible that a threshold of vitamin D must be met before cardioprotective and antihypertensive effects of vitamin D are met, although it’s also likely a whole host of other factors are at play that are likely to interact with RAS and other vascular systems. It’s important to remember that many biological systems are extremely interdependent.
With that being said, given the prevalence of vitamin D deficiency supplementation may be critical irrespective of whether it may be beneficial for hypertension.
It’s important to understand if you are vitamin D deficient, and to address this with medical professionals to seek out methods of dealing with the deficiency.
Although vitamin D is well-tolerated for many, remember that high doses may lead to hypercalcemia which can also have detrimental effects on the body. Again, remember to consult medical professionals and additional resources when judging how to supplement.
Additional articles can be found below for those interested, with some looking at cardiovascular disease or other dysfunctions associated with vitamin D deficiency as well:
Liu, et al.13: Vitamin D and Multiple Health Outcomes: An Umbrella Review of Observational Studies, Randomized Controlled Trials, and Mendelian Randomization Studies.
Latic, N., & Erben, R. G. 14: Vitamin D and Cardiovascular Disease, with Emphasis on Hypertension, Atherosclerosis, and Heart Failure.
Jeong, et al.15: Vitamin D and Hypertension
For now, additional entries in this series may be shelved for a later time. However, the next post in the series will likely look at functional foods and nutraceuticals.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

May, J. M., & Harrison, F. E. (2013). Role of vitamin C in the function of the vascular endothelium. Antioxidants & redox signaling, 19(17), 2068–2083. https://doi.org/10.1089/ars.2013.5205
Guan, Y., Dai, P., & Wang, H. (2020). Effects of vitamin C supplementation on essential hypertension: A systematic review and meta-analysis. Medicine, 99(8), e19274. https://doi.org/10.1097/MD.0000000000019274
Note that many studies on hypertension won’t show dramatic declines when using one intervention alone. This suggests that hypertension should be considered as a disorder with many different factors, albeit with many of these factors being interdependent. Therefore, targeting one area in particular may not show drastic declines in blood pressure.
Scurvy is a disease of severely low vitamin C levels. Many sailors were afflicted with the disease in centuries prior where lack of onboard vitamin C rich foods for long periods caused many sailors to succumb to the disease and die. The main reason for these deaths are due to vitamin C’s role in building collagen, a structural protein found in many parts of the body such as connective tissue. It’s because of this role in collagen construction that scurvy tends to present with bleeding gums and loosened teeth. It’s probably for this reason most portrayals of pirates show them with very bad teeth.
Moser, M. A., & Chun, O. K. (2016). Vitamin C and Heart Health: A Review Based on Findings from Epidemiologic Studies. International journal of molecular sciences, 17(8), 1328. https://doi.org/10.3390/ijms17081328
Morelli, M. B., Gambardella, J., Castellanos, V., Trimarco, V., & Santulli, G. (2020). Vitamin C and Cardiovascular Disease: An Update. Antioxidants (Basel, Switzerland), 9(12), 1227. https://doi.org/10.3390/antiox9121227
Bikle DD. Vitamin D: Production, Metabolism and Mechanisms of Action. [Updated 2021 Dec 31]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278935/
Legarth, C., Grimm, D., Wehland, M., Bauer, J., & Krüger, M. (2018). The Impact of Vitamin D in the Treatment of Essential Hypertension. International journal of molecular sciences, 19(2), 455. https://doi.org/10.3390/ijms19020455
Lin, L., Zhang, L., Li, C., Gai, Z., & Li, Y. (2019). Vitamin D and Vitamin D Receptor: New Insights in the Treatment of Hypertension. Current protein & peptide science, 20(10), 984–995. https://doi.org/10.2174/1389203720666190807130504
Vaidya, A., & Forman, J. P. (2010). Vitamin D and hypertension: current evidence and future directions. Hypertension (Dallas, Tex. : 1979), 56(5), 774–779. https://doi.org/10.1161/HYPERTENSIONAHA.109.140160
Palacios, C., & Gonzalez, L. (2014). Is vitamin D deficiency a major global public health problem?. The Journal of steroid biochemistry and molecular biology, 144 Pt A, 138–145. https://doi.org/10.1016/j.jsbmb.2013.11.003
Chen, S., Gemelga, G., & Yeghiazarians, Y. (2022). Is Vitamin D Supplementation an Effective Treatment for Hypertension?. Current hypertension reports, 24(10), 445–453. https://doi.org/10.1007/s11906-022-01204-6
Liu, D., Meng, X., Tian, Q., Cao, W., Fan, X., Wu, L., Song, M., Meng, Q., Wang, W., & Wang, Y. (2022). Vitamin D and Multiple Health Outcomes: An Umbrella Review of Observational Studies, Randomized Controlled Trials, and Mendelian Randomization Studies. Advances in nutrition (Bethesda, Md.), 13(4), 1044–1062. https://doi.org/10.1093/advances/nmab142
Latic, N., & Erben, R. G. (2020). Vitamin D and Cardiovascular Disease, with Emphasis on Hypertension, Atherosclerosis, and Heart Failure. International journal of molecular sciences, 21(18), 6483. https://doi.org/10.3390/ijms21186483
Jeong, H. Y., Park, K. M., Lee, M. J., Yang, D. H., Kim, S. H., & Lee, S. Y. (2017). Vitamin D and Hypertension. Electrolyte & blood pressure : E & BP, 15(1), 1–11. https://doi.org/10.5049/EBP.2017.15.1.1



https://youtu.be/NgT8I-5NnHU
As always thank you for these great insights.
As you mention a future post on nitric oxide, my favourite source of info has been Beth Shirley. This is a link to a webinar on NO and methylene blue (which you covered really will last year I recall)
There's a lot of research concerning nutrition and health to wade through, isn't there? It can make a person wonder how humanity ever survived without it. Or it might call one to notice how well humanity survived for so long without it.
Is this research actually helping, or is it part of the problem? It doesn't take much research to realize that food and other essentials have changed, especially over the past two centuries, and that general health has declined as well.
It isn't necessary to prove causation before we can begin to take responsibility for our own health. Strangely, I don't find much interest in doing that among the people I know. I wonder what causes that? (Really, I do.)