Managing Hypertension Part I
On balancing mineral levels; not just sodium is a key player in hypertension.
So far we’ve detailed the dangers of hypertension in both the vaccinated as well as in the broader population. It’s likely that many of us will experience hypertension within our lifetime, predominately owed to the poor eating habits and lifestyles of modernity.
The main approach to hypertension takes on a multifaceted approach targeting diet, weight loss, exercise, sleep, stress, and pharmaceuticals if necessary.
Strikingly, the CDC reports that only 1/4 of hypertensive patients have their hypertension well-managed.
Given that hypertension is one of the leading causes of cardiovascular disease and death, there’s a critical need to properly address hypertension and consider ways that people can get it under control.
The next few posts will provide a general outline of non-pharmaceutical approaches to hypertension.
Because it will be near impossible to cover all aspects of hypertension links and relevant information will be provided.
Also, the scope of this review makes this a multipart series. This first part will provide an overview of sodium and how sodium is not the only mineral critical in controlling hypertension.
Select General Articles
To start, here’s a few articles that provide a broad look at nonpharmaceutical approaches to hypertension. Note that the information is not intended to be a guideline, but a general look at some of the information available:
Oza, R., & Garcellano, M.1: Nonpharmacologic management of hypertension: what works?
Fu, et al.2: Nonpharmacologic Interventions for Reducing Blood Pressure in Adults With Prehypertension to Established Hypertension
Mayo Clinic: 10 ways to control high blood pressure without medication
Mahmood, et al.3: Non-pharmacological management of hypertension: in the light of current research
Harrison, et al.4: Pathophysiology of Hypertension
For those who are interested in an overview of how hypertension occurs.
I. Dietary Control of Hypertension
The following takes a functional approach to nutrients whereby some of the mechanisms of actions for plant compounds, ions, and other molecules are outlined for their role in hypertension. Again, a broad approach will be taken with relevant citations provided.
1. Mineral Homeostasis
One nonpharmaceutical approach to hypertension that gets a lot of attention is sodium intake. The over consumption of sodium in most modern diets is a key contributor to the level of hypertension seen in the West, a phenomenon labeled salt-related hypertension. However, it’s not just sodium intake that has changed in the modern diet, but the consumption of all minerals that has been severely altered. Rather than just look at sodium alone, it’s instead a balancing mechanism between sodium and the consumption of other ions such as potassium, magnesium, and calcium that is critical to managing hypertension.
a. Sodium Reduction
Sodium is a critical element for bodily functions, and yet for our ancestors sodium intake may have been relatively low as most food sources did not contain high levels of the mineral.
As noted in a review from Takahashi, et al.5 the low sodium sourced from foods likely contributed to an evolutionary mechanism to retain sodium:
Sodium is the most essential mineral in mammalian physiology. In particular, ingestion of high amounts of sodium salt may be required to keep blood pressure high. As sodium intake is limited in natural foods, a physiological mechanism to prevent sodium loss into urine would have been established early in human evolution. The most powerful mechanism is the RAAS,33, 34, 35 which is maximally activated in people with a minimal sodium intake. In addition, sodium is reabsorbed via the activated sympathetic nervous system, and reabsorption is specifically controlled by renal nerves.36, 37, 38
Therefore, when sodium was sparse mechanisms to retain sodium contributed to our well-being. In modern times with sodium being abundant overconsumption is possible, and no evolutionary mechanism may be available to help properly compensate for the excess sodium.
This is in contrast to other minerals such as potassium, which are likely abundant in fruits and vegetables. Therefore, there was no need for physiological processes to retain potassium (so it is assumed), and therefore the mechanisms did not evolve, thus requiring continuous consumption to keep levels adequate.
The effects of sodium are widespread, usually involving the renin-angiotensin-aldosterone system (RAAS), sodium transporters, and renal mechanisms.
For instance, sodium absorption through ion channels may activate RAAS leading to hypertension via the production of aldosterone and Ang II.
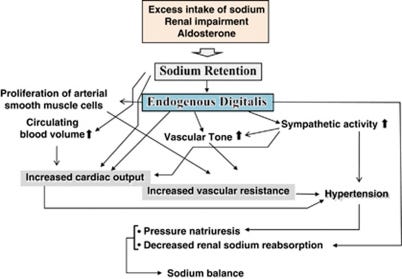
Sodium has many stimulatory effects on the kidneys, which serve as the main site of renin production. Here, sodium and other ions are responsible for the excretion of water (diuresis) and the release of ions (natriuresis).
High water and sodium intake may increase blood pressure, activating diuresis and natriuresis of the kidneys to release fluids and normalize blood pressure. However, high consumption of sodium, as well as altered renal function, may lead to alterations in sodium channel activity, in which sodium is not released but reabsorbed by the body. In reabsorbing sodium water may then be reabsorbed as well, and thus hypertension may be sustained.
Although we aren’t covering pharmaceuticals most diuretics, such as Thiazides, inhibit sodium transporters and prevent the reabsorption of sodium, thus allowing the body to regulate blood pressure more effectively by forcing natriuresis.
Most dietary recommendations suggest limiting sodium intake as one of the main ways of managing hypertension, although we’ll note that the mineral balance is not contingent upon sodium alone, but the dynamics of other minerals as well.
More information can be found in this review from Grillo, et al.:
Grillo, et al.6: Sodium Intake and Hypertension
b. Potassium, Magnesium, and Calcium
In contrast to sodium other minerals such as potassium, magnesium, and calcium help to reduce blood pressure by countering the effects of sodium.

Potassium is one of the main counter ions to sodium, in that high potassium aids in natriuresis and restoration of blood pressure (Palmer, B.F. & Clegg, D.J7):
Mechanistically, increased K+ intake leads to accumulation in the interstitium of the kidney causing an inhibitory effect on the thick ascending limb and to a lesser extent proximal tubular NaCl reabsorption resulting in increased flow and Na+ delivery to the distal nephron [16]. In addition, slight increases in plasma K+ concertation are sensed by cells in the initial portion of the distal convoluted tubule leading to an inhibitory effect on the thiazide sensitive Na+-Cl− co-transporter (NCC). Increased flow and Na+ delivery to the aldosterone sensitive distal nephron (ASDN) stimulates electrogenic and flow mediated K+ secretion. In addition to maintaining a normal plasma K+ concentration, these natriuretic effects contribute to the blood pressure lowering effect of high K+ intake. By contrast, reductions in K+ intake lead to increased activity of NCC and limit K+ secretion by reducing Na+ delivery and flow to the ASDN. The effect of a K+ deficient diet to reduce K+ secretion at the expense of increased Na+ retention has been linked to the pathogenesis of salt-sensitive hypertension.
Potassium also appears to have effects on nitric oxide production which helps to stimulate vasodilation, as well as other mechanisms that reduce hypertension (Houston, M. C., & Harper, K. J.8):
The homeostasis of sodium and potassium plays an important role in endothelium‐dependent vasodilatation. 39 Sodium retention decreases the synthesis of nitric oxide, an arteriolar vasodilator elaborated by endothelial cells, and increases the plasma level of asymmetric dimethyl‐L‐arginine, an endogenous inhibitor of nitric oxide production. 40 a diet rich in potassium as well as increases in serum potassium, even within the physiologic range, cause endothelium‐dependent vasodilatation by hyperpolarizing the endothelial cell through stimulation of the sodium pump and opening potassium channels. 41 In addition, other proposed mechanisms by which potassium can influence BP include natriuresis, modulation of baroreceptor sensitivity, reduced vasoconstrictive sensitivity to norepinephrine and angiotensin II, increased serum and urinary kallikrein, increased sodium/potassium AT Pase activity, alteration in DNA synthesis, and proliferation in vascular smooth muscle and sympathetic nervous system cells. 42 , 43
The significance of sodium/potassium imbalance in hypertension cannot be overstated.
Modern eating habits have heavily altered the ratio of sodium and potassium, much to our detriment. It’s assumed that consumption of sodium is nearly double what is recommended as reported by the American Heart Association9. In contrast, consumption of other minerals such as potassium are several hundred mg short of what should be achieved daily, and that's not taking into account the level of excess sodium that is already being consumed that may need to be countered by high potassium.
Therefore, the effect here is likely twofold in elevating hypertension risk, highlighting the significance of ensuring adequate potassium levels.
For foods rich in potassium potatoes, bananas, leafy vegetables, fruits, and nuts are good sources of potassium. A compendium of potassium-rich foods can be found on The Dietary Guidelines of America website.

When it comes to magnesium, the actual effects of magnesium on hypertension haven’t been elucidated to the same extent as potassium.
Houston, M.C.10 notes some possible mechanisms of magnesium on hypertension, including competing with sodium as well as having synergistic mechanisms with potassium:
One of the mechanisms by which magnesium lowers BP is by acting like a natural calcium channel blocker. Magnesium competes with sodium for binding sites on vascular smooth muscle cells, increases prostaglandin E, binds to potassium in a cooperative manner, induces endothelial‐dependent vasodilation, improves endothelial dysfunction in hypertensive and diabetic patients, decreases intracellular calcium and sodium, and reduces BP. 28 , 29 , 40 Magnesium is more effective in reducing BP when administered as multiple minerals in a natural form and as a combination with magnesium, potassium, and calcium than when given alone. 41
Magnesium is also an essential cofactor for the delta‐6‐desaturase enzyme, which is the rate‐limiting step for the conversion of linoleic acid (LA) to gamma‐LA (GLA). 42 , 43 , 44 GLA, in turn, elongates to form DGLA (dihomo‐gamma‐lineleic acid), the precursor for prostaglandin E1 (PGE1), is both a vasodilator and platelet inhibitor. 42 , 43 , 44 Low magnesium states lead to insufficient amounts of PGE1, causing vasoconstriction and increased BP. 42 , 43 , 44
In addition to BP, magnesium regulates intracellular calcium, sodium, potassium, and pH as well as left ventricular mass, insulin sensitivity, and arterial compliance. 17 , 20 Magnesium also suppresses circulating Na+K+ATPase inhibitory activity that reduces vascular tone. 24
Magnesium is also a mineral that many are not getting enough of due to lack of eating whole foods, and a deficiency has been associated with increased risk of cardiovascular disease akin to high sodium consumption.
Of note, the NIH reports that people may be obtaining only half of the daily magnesium needed, with the groups likely to be the most at risk being men over the age of 70 and both adolescent boys and girls, suggesting that supplementation may be a viable option for some groups.
Good sources of magnesium includes nuts, seeds, dark leafy greens, and dairy. Harvard provides a list of specific foods as well.

Lastly, with calcium there appears to be an association between high levels of calcium and lower blood pressure.
Houston, M. C., & Harper, K. J. notes these effects with calcium:
Resnick 66 has offered 2 possible mechanisms for the various responses to calcium supplementation, discussed in detail below. A reduction in calcium in the diet may cause calcium depletion from all membrane storage sites, resulting in less stability of the vascular smooth muscle cell membrane. 67 When present in optimal concentrations, calcium stabilizes vascular cell membranes, inhibits its own entry into cells, and reduces vasoconstriction. 42 Calcium works in combination with other ions such as sodium, potassium, and magnesium to provide an ionic balance to the vascular membrane, vasodilatation, and resulting reduced BP.
Calcium deficiency is likely to be less common than other mineral deficiencies due to fortification of foods and dairy being a good source.
Calcium can be found predominately in dairy, as well as greens and nuts.
Essentially, many whole foods rich in one mineral is likely to be rich in other minerals, suggesting that mineral deficiency is likely to be caused by lack of whole, nutrient-dense foods.
c. Contraindications with Blood Pressure Medications
For those who are experiencing a mineral deficiencies a word of caution is needed when supplementing while on blood pressure medications.
Note that many medications may lead to retention of minerals, and therefore a disease of too much potassium (hyperkalemia) too much magnesium (hypermagnesemia), or too much calcium (hypercalcemia).
In the case of potassium the use of drugs such as ARB’s, ACE inhibitors, and some diuretics may lead to hyperkalemia. Therefore, it’s important to take care in taking mineral supplementations when on specific blood pressure medications.
Note that excess levels of potassium, magnesium, and/or calcium can also contribute to cardiovascular disease risk, again emphasizing the importance of balance.
It’s important to discuss with a healthcare provider when trying to navigate proper medication use as well as supplementation or consumption of mineral-rich foods.
More and more it becomes apparent that reduction in sodium is not the only way to deal with hypertension. Studies have alluded to the fact that both low potassium and sodium can contribute to cardiovascular disease, while elevated magnesium and calcium levels can contribute as well.
Rather than looking at sodium alone, it’s the net effect of free minerals that contribute to the overall reduction in blood pressure.
By all accounts it would appear that the best way to address hypertension would be to reduce sodium increase consumption of whole foods. However, in cases when foods may not be enough supplementation may be warranted.
More importantly, care should be taken when supplementing or eating mineral-rich foods while also on antihypertensive medications. Make sure to consult with medical professionals in order to find the best approach when considering mineral supplementation, or really any changes in diet meant to address hypertension.
The next post will focus on vitamins and micronutrients such as fish oil and flavonoids.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

Oza, R., & Garcellano, M. (2015). Nonpharmacologic management of hypertension: what works?. American family physician, 91(11), 772–776.
Fu, J., Liu, Y., Zhang, L., Zhou, L., Li, D., Quan, H., Zhu, L., Hu, F., Li, X., Meng, S., Yan, R., Zhao, S., Onwuka, J. U., Yang, B., Sun, D., & Zhao, Y. (2020). Nonpharmacologic Interventions for Reducing Blood Pressure in Adults With Prehypertension to Established Hypertension. Journal of the American Heart Association, 9(19), e016804. https://doi.org/10.1161/JAHA.120.016804
Mahmood, S., Shah, K. U., Khan, T. M., Nawaz, S., Rashid, H., Baqar, S. W. A., & Kamran, S. (2019). Non-pharmacological management of hypertension: in the light of current research. Irish journal of medical science, 188(2), 437–452. https://doi.org/10.1007/s11845-018-1889-8
Harrison, D. G., Coffman, T. M., & Wilcox, C. S. (2021). Pathophysiology of Hypertension: The Mosaic Theory and Beyond. Circulation research, 128(7), 847–863. https://doi.org/10.1161/CIRCRESAHA.121.318082
Takahashi, H., Yoshika, M., Komiyama, Y., & Nishimura, M. (2011). The central mechanism underlying hypertension: a review of the roles of sodium ions, epithelial sodium channels, the renin-angiotensin-aldosterone system, oxidative stress and endogenous digitalis in the brain. Hypertension research : official journal of the Japanese Society of Hypertension, 34(11), 1147–1160. https://doi.org/10.1038/hr.2011.105
Grillo, A., Salvi, L., Coruzzi, P., Salvi, P., & Parati, G. (2019). Sodium Intake and Hypertension. Nutrients, 11(9), 1970. https://doi.org/10.3390/nu11091970
Palmer, B.F., Clegg, D.J. Blood pressure lowering and potassium intake. J Hum Hypertens 34, 671–672 (2020). https://doi.org/10.1038/s41371-020-00396-1
Houston, M. C., & Harper, K. J. (2008). Potassium, magnesium, and calcium: their role in both the cause and treatment of hypertension. Journal of clinical hypertension (Greenwich, Conn.), 10(7 Suppl 2), 3–11. https://doi.org/10.1111/j.1751-7176.2008.08575.x
The AHA reports that most Americans are eating around 3,400 mg of sodium per day, while the AHA recommends around 2,300 mg limit with an ideal 1,500 mg marker.
Houston M. (2011). The role of magnesium in hypertension and cardiovascular disease. Journal of clinical hypertension (Greenwich, Conn.), 13(11), 843–847. https://doi.org/10.1111/j.1751-7176.2011.00538.x


sodium reduction produces week results.
From the study "Thirty four trials (3230 participants) were included. Meta-analysis showed that the mean change in urinary sodium (reduced salt v usual salt) was -75 mmol/24 h (equivalent to a reduction of 4.4 g/day salt), and with this reduction in salt intake, the mean change in blood pressure was -4.18 mm Hg (95% confidence interval -5.18 to -3.18, I(2)=75%) for systolic blood pressure and -2.06 mm Hg (-2.67 to -1.45, I(2)=68%) for diastolic blood pressure."
Reducing salt intake by a whopping 4.4 g/day produced a mere 4.18 mm hg reduction in systolic and a 2.06 in diastolic. That's a lot of bland food for a benefit that is barely worth considering
Good research but IRL sodium reductions doesn’t do much unless someone already had renal dysfunction or CHF.
Instead of looking at the minerals as the cause, perhaps look at what low or high levels do to the body in terms of the hormonal or signaling responses.
In a normal person, if they eat a lot of sodium foods their kidneys can easily clear it without a problem.
As we can’t manufacture sodium we need sodium and all the other minerals in our diet. Our kidneys are there to help clear out excess which they do very well.
I don’t have the link handy but I believe All Cause Mortality is highest in people on low sodium diets. So the general recommendations of lowering sodium intake is not helpful unless someone has preexisting renal dysfunction or CHF.
As for the main cause of hypertension I see in clinical practice, it is chronic insulin resistant states that occur most often in overweight people on the SAD diet.
As insulin rises we store more fat. When we store fat we need to balance it with water and minerals including sodium. So chronic high insulin states makes us retain more salt water which can feedback to the kidneys and contribute to elevated blood pressure.
I rarely recommend low salt diets but I do agree to get healthy amounts of the other minerals you discussed.
Last thing.
What is the bodies response if we don’t have enough sodium? Our hormones adjust to increase our blood pressure. In other words in a low or deficient sodium state our body raises our blood pressure. Perhaps in high insulin states sodium is partitioned more in fat cells so the kidneys think we need more??? Just a hypothesis??