Is it a weakened immune system?
A brief assessment of the "weakened immune system" post-vaccination study.
Apologies for the delayed posting of this article. I had some things going on over the weekend, and last minute found out someone was going to be visiting and had to scrambled to do some additional cleaning/organizing. As a heads up, if anyone is traveling this holiday season PLEASE alert friends and family weeks in advance, not DAYS!
Anyways…
This study1 has gotten a lot of attention for a possible conclusion of weakened immune systems post-vaccination, and more alarmingly a possible risk in children that hasn’t been studied before.
The prior article raised some food for thought, although it was initially intended to be an assessment. I guess my thoughts went down different routes and I wanted to organize them.
But here we’ll take a brief look and see what the study entails, while also adding some more context if needed.
Study Outline
This study in question is a rather small one, utilizing patients who were part of another study on the BCG vaccine as noted in the prior article. Remember that this study, the Melbourne Infant Study: BCG for Allergy and Infection Reduction (MIS BAIR), was conducted in neonates in which the BCG vaccine, a live, attenuated vaccine against tuberculosis, was given to one group of children while another was given placebo. The children were then tracked for a given time period to see the rates of secondary infections, allergies, and asthma. It essentially acted as a more tame version of assessing “all-cause mortality reductions” from other vaccines.
Nearly 2/3 of the children enrolled in the COVID vaccine/cytokine study were in the placebo group. Again, the nature of this point is not clear to me. However, given that we are examining all of these vaccination procedures from the lens that they may influence immune responses down the line, this is something to at least think about when interpreting this information.
The authors do make a note in which separating out BCG recipients from BCG non-recipients did not appear to result in greater differences in results:
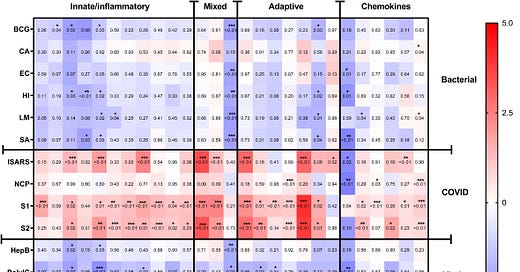
A sensitivity analysis of only participants who did not receive BCG vaccination in MIS BAIR indicated that BCG status had a negligible or no effect on the reported effect of BNT162b2 vaccination on cytokine responses (Supplementary Figure S3).
Children who were assessed for cytokine responses post-vaccination were administered the Pfizer/BioNTech vaccine, being provided 2 doses at 8 weeks apart.
Because no control group was used as it was deemed “unethical” to not vaccinate children against COVID the children were used as their own control, with blood samples taken the day prior to or the day of the first vaccination (V1). A second sample was then taken around 4 weeks after the second dose (V2+28). Children were then also given the option to provide an additional blood sample 6 months later (V2 + 182).
However, attrition seemed high relative to the 6-month follow-up, with the initial 29 children included in the study dropping down to 8 by the V2 + 182 optional sample collection timepoint.
Also, bear in mind that the caption for Supplementary Figure S3 notes that the heatmap constructed for BCG non-recipients comprised 25 participants. If following the numbers, this seems to suggest that only 4 of the included participants received the BCG vaccine.2
Blood samples were then challenged with different antigens/pathogens of either viral or bacterial origin. For bacteria, nearly all bacterial strains were heat-killed bacteria aside from BCG which, again, is a live, attenuated bacterial strain that causes tuberculosis.
For SARS-COV2 both inactivated virus (iSARS) as well as viral antigens were used, including the nucleocapsid protein (NCP).
In regards to other “viral” agents the story is a little bit more complicated. Note that no inactivated viruses were used for the “virus” part of the study. In actuality, the only virus that was used was a surface antigen derived from Hepatitis B. The other two agents are toll-like receptor agonists that are intended to mimic a viral infection, possibly by way of mimicking viral genetic material by way of sharing homology to nucleotides.
For instance, Resiquimod, or R484 is a TLR-7/8 agonist with a ring structure that mimics purines:

Resiquimod appears to be a strong antiviral agent, as its structure is similar to RNA molecules and can induce strong inflammatory responses.
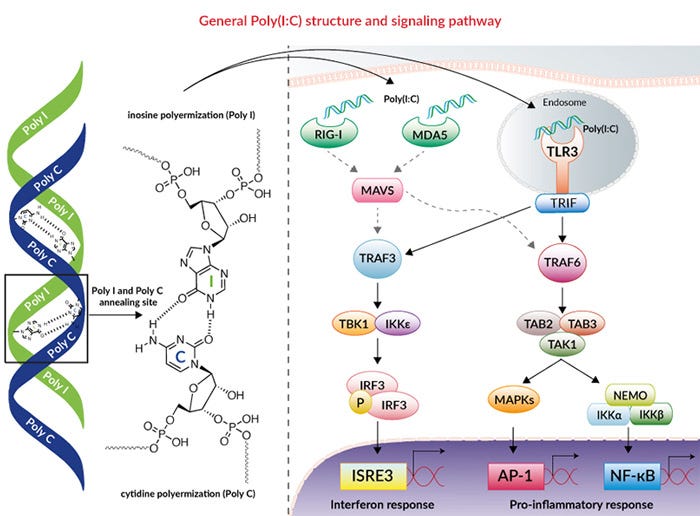
Poly(I:C) is also a toll-like receptor agonist for TLR-3, and its structure mimics that of double-stranded RNA as it is comprised of two chains, with one of Inosine residues and the other of Cytosine residues:
This is important to note because the mRNA vaccines contain N-methylated pseudouridine along with other alterations which make the mRNA undetectable to the immune system. It’s been suggested that the mRNA vaccines reduce toll-like receptor responses, and it may be due to the fact that they go unrecognized.
Now, that being said, the problem is rationalizing whether any weakened response to TLR agonists is due to TLR inhibition of some sort, or due to lack of training of the immune system when it comes to recognition of exogenous RNA. Again, remember that the intent here is to not look at this study alone, but to look at it within the context of trained immunity as a general concept.
Note that this study never uses any actual attenuated or inactivated viral agents aside from SARS, so it’s not really an examination of viral infections but mere proxies by way of exposing blood to a viral antigen or simulacrums of viral genetic material.
Results
With everything said, the results are rather interesting. Across all cytokine measures there appeared to be a supposedly dampened response to bacterial and “viral” agents in children 4 weeks post-vaccination relative to their starting measures.
This can be seen in the heatmaps. Others have shown the cytokine graphs but I think the heatmaps organize things a bit better for assessments.
Heatmaps are more qualitative in their presentation. For this heatmap, agents are shown in rows with corresponding cytokine responses shown in columns labeled on the bottom of the heatmap. The top label denotes cytokines related to innate, adaptive, or mixed immune responses. Different cytokine responses relative to the initial timepoint is color-coded, with more red boxes suggesting a stronger response relative to baseline. More blue colors are associated with a weaker response. A white box notes a possibly minimal change in the cytokine relative to baseline.
Be careful of the numbers within each box, as the numbers are associated with p-values and not the actual heatmap value. Asterisks within each box notes statistical significance and to what degree (i.e. one asterisk is a p-value < .05, two is p-value < .01, etc.).
In a general sense, you want to look for “redder is better” and “bluer is…” I don’t have a rhyme for bluer that is associated with “worse”, but note that more blue is suggestive of a weaker cytokine response relative to baseline. The measures are based on differences between baseline and post-vaccination responses. Note that the values are logarithmic, and so every increase in scale is by a factor of 10 (i.e. a log value of 2 is 10^2 or 100 magnitude difference, not 20).
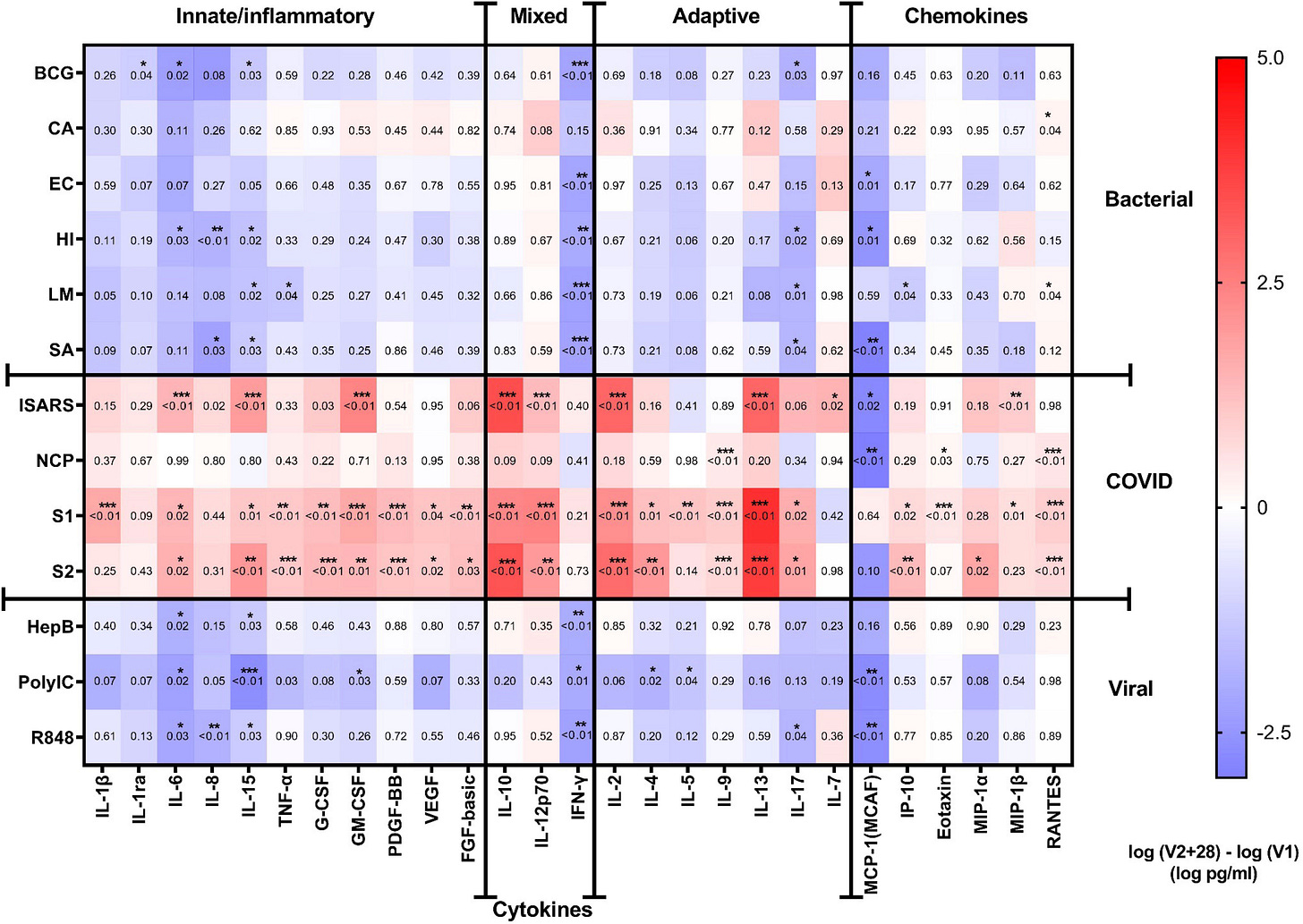
Across the board what’s obvious is that responses to SARS-COV2 (the COVID rows) are stronger relative to baseline at 4 weeks post-vaccination aside from responses to the nucleocapsid protein. However, for all other agents the response appears to be mixed-reduced overall as noted by all of the blue. Note that the difference didn’t appear statistically significant aside from clear examples such as IFN-gamma, MCP-1, and a few interleukins (6, 8, and 15 in particular).
The researchers make the following comments:
Following heterologous bacterial, fungal and viral/TLR agonists stimulation, there was a general decrease in cytokine and chemokine responses in children between V1 and V2 + 28. The largest decreases were seen for IFN-γ and MCP-1 (Figures 2, 3A-C). IL-6, IL-15, IL-17 also decreased between V1 and V2 + 28 following stimulation with BCG, H. influenzae, S. aureus, hepatitis B antigen, poly(I:C), and R848 (Figure 3B). L. monocytogenes stimulation induced IL-15, TNF-α and IP-10 decreases between V1 and V2 + 28 (Figure 3C). IL-8 responses also decreased between V1 and V2 + 28 following H. influenzae and S. aureus stimulation. RANTES was the only analyte that increased in response to heterologous stimulants (L. monocytogenes and C. albicans) between V1 and V2 + 28.
Again, this may seem rather alarming, and in some sense may be suggestive of reduced immune function post-vaccination. However, note that this study is examining cytokine responses rather than immune responses. It’s more that the immunological responses are inferred based on the cytokines, although it doesn’t tell us much of what is actually happening.
It’s worth considering whether the recent presentation of spike may show a stronger response towards spike because the body has been alerted to look out for this antigen in particular. In that regard, immune cells and signaling responses may be biased towards a response that favors spike. This may account for why TLR agonists don’t appear to show a strong response because the immune cells may have not have been trained to survey for that factor in particular.
That being said, the last comment would require an assessment of each child’s prior history to understand the influence of prior infections on overall responses. Keep in mind that any child that tested positive for the NCP was excluded from analysis, including those who tested positive in between the V2+28 and V2+182 timepoints.
Note that the study is a comparative study as well. It doesn’t tell us much about what the reduced cytokine response amounts to in actual individuals since no quantitative measures are provided. It’s possible that the reduced response is still enough to combat pathogens, or that children in general may not produce strong responses to certain antigens. As an example, what would the proper response to Hep B antigen presentation be in children, or for other viral/bacterial antigens?
One positive for this study is that children were matched to their baseline values, but that doesn’t help much when their overall values are jumbled together with the other children, so we don’t know the degree of variability among each child in their responses.
The 6-month follow up is a bit interesting in some aspects. Note that this follow-up only included 8 children relative to the 29 at the 4 week mark, however it appears that the researchers took this into account.
The top heatmap shows differences in cytokine responses 6 months out from the second vaccination (V2+182) when compared to baseline. The bottom heatmap shows difference between the two timepoints post-vaccination (V2+182 compared to V2+28).
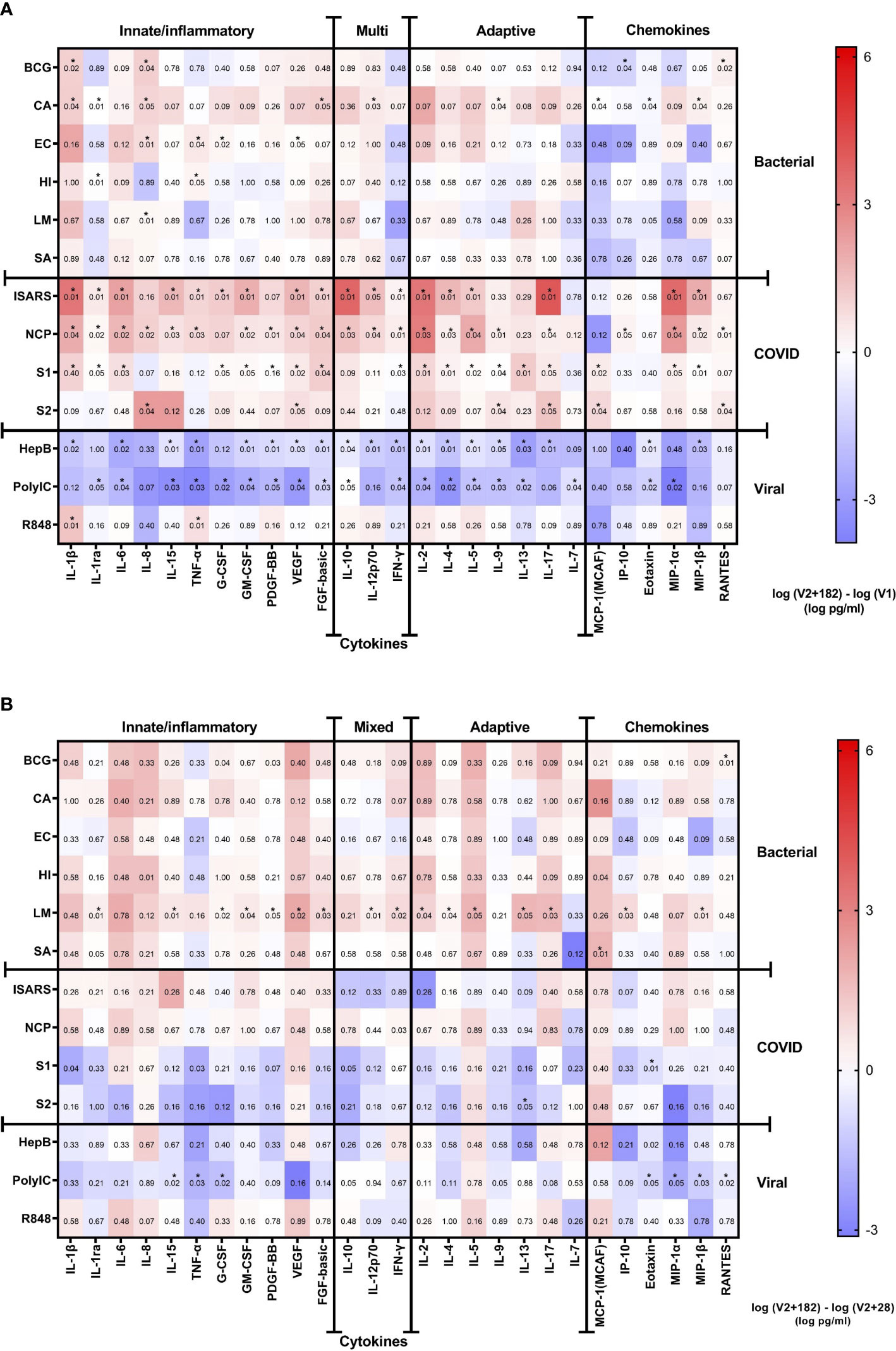
There’s a bit going on here. The best way to parse the two heatmaps is to understand what they are conveying. Essentially, the top heatmap could be seen as a “return to baseline” map. It allows you to see whether cytokine responses normalize 6 months out from vaccination, or whether immunological changes persist and to what degree the changes have manifested.
In contrast, the bottom heatmap is more of a measure of relativism in regards to whether children improved or worsened in the following months. For instance, any blue would suggest that the cytokine response towards that agent may have worsened over time whereas any red may show improvement over time.
A good rationalization would be the response to S1 and S2 of the spike. Note that, overall, the cytokine response to spike is elevated relative to baseline even 6 months post-vaccination. However, when looking at the bottom heatmap the two rows for S1 and S2 appear blue, suggesting that the cytokine response seems to attenuate over time. So even though the response is stronger post-vaccination (as would be expected), it still declines the further out from vaccination one goes (allegedly).
In this case, a discrepancy between bacterial and viral agents appears to have occurred, such that cytokine responses to bacterial agents seems to have “normalized” at the 6 month post-vaccination mark, as noted by the white boxes.
In contrast, the “viral” rows appear blue even at the 6-month mark, noted reduced cytokine responses to these agents months out from vaccination. When compared to the bottom heatmap, note that the values for HepB antigen and PolyIC are blue, suggesting that the response worsened the further out from vaccination one goes (using only two timepoints).
Now, the obvious question is why such a discrepancy is occurring between bacterial and viral agents. The obvious suggestion is that differences in presentation of pathogens may be at play as was noted in the previous article, such that whole bacterial agents as well as the live, attenuated BCG vaccine may provide a more well-rounded cytokine response in contrast to the possibly more selective nature of the HepB antigen and the PolyIC agent. However, given the limitations of this study this is mere speculation. Further studies with different agents may provide a better window into what exactly is going on here.
What does this all mean?
The burning question is whether these results relate to anything meaningful in the real world.
Unfortunately, to that the answer falls along the lines of either “I don’t know” or “it depends”.
Because this study lacked any controls we can’t say for certain whether these results are related to the vaccines or whether these results may be due to seasonal changes in virus and bacteria exposure.
Brian Mowrey makes this remark in his article about this study:
Great, Vaccine Doom Confirmed, except for the thing that I find unhelpful about all these studies — there is no unvaccinated control group. It goes without saying that had there been such a control group, with kids who do not receive the vaccine but are sampled at similar time-points somehow producing similar results, we would need to look to a different explanation (e.g., local seasonal patterns in viruses and bacteria). I will never be satisfied by post-vaccine group biological response studies that leave out controls (and cannot help but think the intention is to get random assay noise past peer review).
Remember that the children in these studies are not isolated during the time between vaccinations and post-vaccinations, and so these children have likely come across various viral and bacterial agents outside of SARS-COV2, which may have influenced their immune responses, especially given that these children are of school age. Although the researchers controlled for SARS-COV2 positivity by excluding children who tested positive for the NSP, the same can’t be said for other pathogens.
And so the study itself becomes paradoxical, whereby the assumption that the mRNA vaccines may alter children’s immune responses has to be considered within the context that other agents may also alter immune responses as well.
So is all of this due to the vaccine in particular, due to circulating pathogens, or due to other circumstances not considered in this study?
There’s also the fact that cytokine responses infer immune responses, but they don’t tell us exactly what else is going on. Note that the adenoviral-based vaccine study3 cited by Noé, et al. looks at monocyte “behavior” as well as cytokine responses, providing a better window into what exactly is going on.
A more detailed assessment would look at each individual cytokine, in particular the ones that showed the greatest variability, and determine what role those cytokines play and what may lead to their reduced release. MCP-1, which seems to be reduced even at 6 months post-vaccination, is an agent that attracts other immune cells and is predominately released by monocytes and macrophages, and may be something worth investigating.
Overall, the missing factor is determining what all of this means in the grand scheme of things.
On one hand, these results may tie into increased infection in children in recent years. However, it doesn’t quite explain whether children should recover or if they should eventually succumb to their illnesses.
This is one of the problems with the narrative of COVAIDS or VAIDS, as it essentially becomes self-contradictory. Consider that AIDS, if left untreated, results in further immune deficiency and worse outcomes for even common pathogens. Most AIDS patients appear to die from secondary infections.
Invocation of COVAIDS or VAIDS should, if the model is being consistent, suggest that people are getting more sick and would require hospitalization or may result in death, and this does not appear to be the case.
Any severe adverse reaction or death post-vaccination doesn’t appear to be related to secondary infections, although the role of HHV reactivation is something worth considering for some individuals.
But even with that being said, the reactivation of VCV for most individuals appeared relatively transient and cleared up without any treatment for most people, again suggesting that there’s more to the immune deficiency than perpetual VAIDS, otherwise we should not expect resolution of VCV reactivation or other illnesses.
We don’t know whether the children included in this study reported various illnesses during the study period, and no reported cases of hospitalizations or exclusions due to death were reported, so once again all of these hypotheticals are still up in the air.
In a more optimistic sense, I’m inclined to consider that people may be more susceptible to infections within the periods following vaccinations, with infections eventually resulting in attenuated of these deficiencies, but again studies would need to further examine what is going on.
Remember that our immune systems are a lot more complex than we may think. There’s still a lot that has not yet been discovered. Consider that the concept of “an innate immune system” seems to be incorrect based on recent findings, and so even a long-held belief in immunology is likely to need some major correcting.
In any case, further studies and real-world corroborations would help discern the degree of meaningfulness from this study.
Substack is my main source of income and all support helps to support me in my daily life. If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists such as myself to provide work outside of the mainstream narrative.

Noé A, Dang TD, Axelrad C, Burrell E, Germano S, Elia S, Burgner D, Perrett KP, Curtis N and Messina NL (2023) BNT162b2 COVID-19 vaccination in children alters cytokine responses to heterologous pathogens and Toll-like receptor agonists. Front. Immunol. 14:1242380. doi: 10.3389/fimmu.2023.1242380
BCG sensitivity analysis of cytokine responses to whole‐blood stimulations 28 days after BNT162b2 vaccination. The mean of the pre- (V1) and post- (V2 + 28) cytokine differences from 25 study participants with no BCG vaccination is plotted in the heatmap colour gradient, with red representing increases and blue indicating decreases.
Murphy, D. M., Cox, D. J., Connolly, S. A., Breen, E. P., Brugman, A. A., Phelan, J. J., Keane, J., & Basdeo, S. A. (2023). Trained immunity is induced in humans after immunization with an adenoviral vector COVID-19 vaccine. The Journal of clinical investigation, 133(2), e162581. https://doi.org/10.1172/JCI162581






Yet another vaccine study without a real control group. Is there even a single vaccine study that tests against an unvaccinated control group?
Only in kids and a very small group over very short time period... but how else do they keep the money coming in? Gotta think up something to study. I think it's not been long enough to give any indication of long term immune dysfunction. The clinician and parents will be able to tell over time if their kids are less healthy. And we can see what happens in those we know.
Off topic but did you comment anywhere on the findings out of Japan where they tried tracing covid back via sequencing and came to the conclusion that every variant has come from a lab and is not a "natural" variant? Sometimes I overwhelm myself with too much reading and can't recall who wrote on what :|)
Thank you for your time doing all this - I do enjoy your dismantling of the headlines. In this crazy world it's too easy to just skim.