Did "Trump's" Hydroxychloroquine kill thousands of people?
Or are absurd claims based on absurd evidence?
For a tl;dr:
Recent articles have reported on a new study suggesting that the use of HCQ for COVID has been associated with deaths of thousands of individuals, with some of these outlets using such numbers to blame Trump for these deaths.
However, the data used appears to have many problems:
Although hospitalization rates for COVID are derived from a collective database, the mortality rate and HCQ prescription rate are derived from select studies, meaning that the true rate of mortality and HCQ prescription among countries is unknown and only estimated. This is even worse for countries such as Belgium, in which estimates were based solely on one observational study.
The Odds Ratio is derived from estimations pertaining to two studies specifically (WHO SOLIDARITY and RECOVERY), and thus may not be reflective of the actual increased risk of mortality from HCQ administration. This is also complicated by the fact that these studies looked at hospitalized patients in particular, adding additional confounders for other comorbidities in real-world administration.
Because the excess mortality rate is derived from the variables outlined above it’s hard to trust that the estimated values are accurate. The authors themselves appear to show uncertainty in their findings, and yet seem to also double down on their “thousands of excess deaths claims”.
The media is, of course, running with this narrative even though the data is highly suspect- don’t fall for such media trickery!
A recent analysis1 published within the journal Biomedicine & Pharmacotherapy has thrown Hydroxychloroquine back into the media spotlight. This time, remarks from the study appear to suggest that over 17,000 excess deaths from early 2020 may have been related to use of Hydroxychloroquine.
This has led to varying headlines, with one published in Forbes bearing the most critical title:
Although Newsweek’s headline isn’t much better:

A rather damning headline if true, and various outlets have also taken to reiterating the 17,000 number while not alluding to Trump in particular.

The timing of this study couldn’t be any more…timely as Trump is met with further political turmoil, making this report pertinent to an anti-Trump narrative.
However, what’s important is determining whether the claims made by such a study are of merit, or whether there may be things worth critiquing.
First off, it’s rather interesting that the study comes with the following title:
“an estimate”- an interesting phrase to include in the title. The summary of the findings can be found in the following infographic. Take note of how excess deaths are calculated and the variables that were used:
It’s the last column where the “17,000 deaths” were derived from, and It’s the origins of these numbers that are worth scrutinizing. We’ll look at some of the origins and some of the problems with these numbers, and why it’s likely a far stretch to make such claims as the mainstream press are making.
Note here that Pradelle, et al. got its COVID hospitalization numbers from the database of various countries:
We obtained the total number of hospitalisations by country from the dedicated databases [13], [14], [15]. We used hospitalisation data from the beginning of the pandemic in each country (mostly from March 2020 onward) until 17th July 2020 (i.e. date of publication of the RECOVERY trial[5]).
However, the mortality rate and HCQ prescription rates for each country were derived from reviews of several studies, with the mortality rate for the US being derived specifically from a collection 20 studies. In contrast, Belgium’s mortality rate and HCQ prescription was derived from one scant study:
The mortality rates for each country were estimated using a meta-analytic approach by pooling (random-effects model) the proportions reported in all included cohort studies. The HCQ exposure was estimated using median and extreme estimates from the same systematic review. A sensitive analysis was conducted using the estimate of mortality rate in hospitalised patients from other sources such as national surveillance report and regionwide analysis.
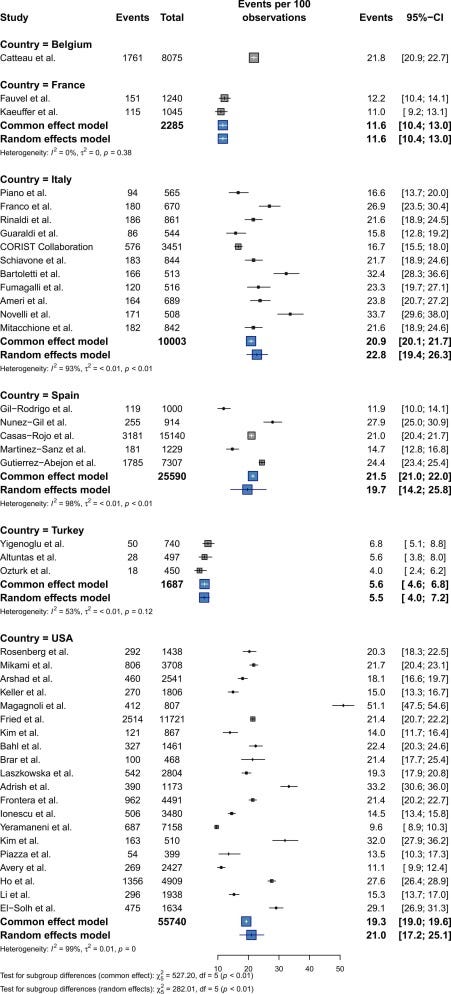
Note that several of these studies were not designed to look at mortality related to administration of Hydroxychloroquine but made note of Hydroxychloroquine use for different patient demographics. For instance, one US study compared mortality outcomes in cancer patients relative to non-cancer patients.2 Another included study looked at outcomes in smokers relative to non-smokers.3
That is to say, the included studies for the analysis of mortality were not derived from studies looking into HCQ use as a primary outcome, and instead were designed to look at other variables with the use of Hydroxychloroquine being tangential to the studies’ primary objectives. Although the mortality rate used for this study was intended as a general value based on the available studies, it’s also worth considering that these calculated mortality rates are likely to be heavily skewed by the included studies, which may be confounded by other factors, making these mortality rates possibly unreliable. Note that the range of mortality for the studies included for the US alone are 9.6% up to 33.2%.
It’s also strange that the authors appear to use hospitalization rates derived from a database but do not report mortality rates or HCQ prescription from that database as well. This is likely due to privacy concerns; however, it also points to the fact that the numbers being used are derived from different populations and being applied to a group that may not be reflected in the calculated mortality and HCQ prescription rates.
What’s also strange is the Belgian study which was included to report the 21.8% mortality rate. The study itself, from Catteau, et al,4 was an observational study which looked at low-dose administration of HCQ in COVID hospitalized patients, with their findings ironically suggesting that use of HCQ resulted in lower mortality rates when compared to those not provided HCQ, with the results noting a 17.7% mortality rate among HCQ patients as compared to the 27.1% mortality among the non-HCQ group, with the authors making the following remarks in their Discussion:
In this large analysis of patients admitted for COVID-19 in Belgium, HCQ monotherapy administered at a dosage of 2400 mg over 5 days was independently associated with a lower in-hospital mortality rate compared with patients treated with supportive care only, even after adjustment for age, major co-morbidities and disease severity at admission. Importantly, mortality was reduced regardless of the time from symptom onset to diagnosis and HCQ treatment initiation.
Again, ironic that mortality data suggesting that this Belgian cohort saw reduced mortality with HCQ would be used in a study to denote excess mortality related to HCQ.
The next issue stems from the Odds Ratio (OR) used in this study. The OR is rather critical to this study as it serves as the “excess mortality” multiplier. As in, the OR is used to suggest that mortality outcomes in those provided HQC may be skewed more towards death relative to those who were not provided HCQ. In this case, the OR was derived from a prior meta-analysis from Axfors, et al.5 which looked at OR values from various studies to come up with a generalized OR used by Pradelle, et al.
Note here that two drivers for the overall OR are the WHO SOLIDARITY and the RECOVERY trial:
Barring criticisms of the SOLIDARITY and RECOVERY clinical trials, it tells us once again that the data used to calculate the OR may itself not be reflective of a broader population. More importantly, it tells us that the pool of participants used to estimate the mortality rate and HCQ prescription rate may not be synonymous with the group used to calculate the OR. This is made worse because the OR is driven predominately by the RECOVERY and the WHO SOLIDARITY trials.
It's all heterogeneous and unreliable
Overall, what these factors suggest is that the 17,000 deaths related to HCQ are, as the title suggests, merely estimates. However, due to the means in which the excess mortalities were calculated it’s likely that these values are wildly inaccurate estimates. The heterogeneity of the mortality rates and HCQ prescription rates means that we don’t know how similar these values are to the actual rates for the hospitalized patients used as the general population from which the excess death calculations were made. The OR itself may be unreliable because this value is derived from only two RCTs. By pairing these values (mortality/prescription rates and the OR) together it’s highly unlikely that the result is going to be accurate.
Consider the fact that the authors consider one large limitation in their study being the uncertainty of HCQ’s effect on patient mortality:
Fourth, we did not use all sources of uncertainties related to variables included in the models. We only included variables related to the HCQ treatment effect. Thus, HCQ-related deaths may be considerably over- or under-estimated. Indeed, the 95% confidence interval of the OR of all-cause mortality related to HCQ ranged from 2% to 20%. In other words, our results might be overestimated by a factor 5 (i.e. the actual number of deaths related to HCQ would be ≈3000 deaths) or underestimated by a factor 2 (i.e. the actual number of deaths related to HCQ would be ≈30000 deaths). Thus, the effect of HCQ on mortality was the main source of uncertainty for the proposed estimates.
Of course, the authors may get away with inaccuracies by claiming their study is “an estimate”, although this hasn’t stopped the authors from still suggesting that their findings are likely to be an underestimate, and that this information should bar off-label use for future pandemics:
The main finding of the present study is that HCQ might have been associated with an excess of 16990 deaths during the first wave of the COVID-19 pandemic in the six countries for which data were available. Given that reliable data on hospitalizations, HCQ use and in-hospital mortality for most countries, these numbers likely represent the tip of the iceberg only thus largely underestimating the number of HCQ-related deaths worldwide.
…
Our study showed a high proportion of prescriptions for HCQ even in countries which have restricted its use [84]. This result argues in favour of tightly regulating access to off-label prescriptions during future pandemics [87].
And this hasn’t stopped mainstream outlets from using these estimates to start forming their own narratives that Trump may have led to these excess deaths.
This comment is made even more nonsensical given the fact that all these studies are based upon data from hospitalized patients. It’s not as if hospitals or certain geographic regions in the US just happened to continue using HCQ due to following Trump’s rhetoric.
And even worse, studies such as this one may be used to indict outpatient use of HCQ for COVID, even when none of these studies included to make the 17,000 excess estimate themselves do not provide any information regarding extrapolation for an outpatient setting.
The RECOVERY study6 itself includes a disclaimer suggesting that the study cannot be used to infer outpatient results:
These findings indicate that hydroxychloroquine is not an effective treatment for hospitalized patients with Covid-19 but do not address its use as prophylaxis or in patients with less severe SARS-CoV-2 infection managed in the community.
Axfors, et al. also makes this distinction with their meta-analysis:
We found that treatment with hydroxychloroquine is associated with increased mortality in COVID-19 patients, and there is no benefit of chloroquine. Findings have unclear generalizability to outpatients, children, pregnant women, and people with comorbidities.
As Dr. Steve Risch has mentioned before hospital data regarding HCQ and COVID outcomes are being used to drive outpatient guidelines even though no evidence is there to dissuade the use of HCQ. This is policy being dictated by inconsistencies, with a large reliance on many narrative pushers to be none the wiser to these limitations.
Note that I’m not arguing for or against the use of HCQ for COVID, but rather any argument made for or against its use should be based on relevant data, and it’s quite clear that mainstream outlets and public health officials are obfuscating any sense of nuance by conflating outpatient and inpatient use of HCQ, as well as conflating mortality with HCQ and mortality from.
The data presented in Pradella, et al. is far too messy to make any conclusions, and we should be critical of those who use such messy data for political means.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists such as myself to provide work outside of the mainstream narrative.

Pradelle, A., Mainbourg, S., Provencher, S., Massy, E., Grenet, G., & Lega, J. C. (2024). Deaths induced by compassionate use of hydroxychloroquine during the first COVID-19 wave: an estimate. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie, 171, 116055. Advance online publication. https://doi.org/10.1016/j.biopha.2023.116055
Gagandeep Brar et al., COVID-19 Severity and Outcomes in Patients With Cancer: A Matched Cohort Study. JCO 38, 3914-3924(2020). DOI:10.1200/JCO.20.01580
Adrish M, Chilimuri S, Mantri N, et al Association of smoking status with outcomes in hospitalised patients with COVID-19 BMJ Open Respiratory Research 2020;7:e000716. doi: 10.1136/bmjresp-2020-000716
Catteau, L., Dauby, N., Montourcy, M., Bottieau, E., Hautekiet, J., Goetghebeur, E., van Ierssel, S., Duysburgh, E., Van Oyen, H., Wyndham-Thomas, C., Van Beckhoven, D., & Belgian Collaborative Group on COVID-19 Hospital Surveillance (2020). Low-dose hydroxychloroquine therapy and mortality in hospitalised patients with COVID-19: a nationwide observational study of 8075 participants. International journal of antimicrobial agents, 56(4), 106144. https://doi.org/10.1016/j.ijantimicag.2020.106144
Axfors, C., Schmitt, A.M., Janiaud, P. et al. Mortality outcomes with hydroxychloroquine and chloroquine in COVID-19 from an international collaborative meta-analysis of randomized trials. Nat Commun 12, 2349 (2021). https://doi.org/10.1038/s41467-021-22446-z
RECOVERY Collaborative Group, Horby, P., Mafham, M., Linsell, L., Bell, J. L., Staplin, N., Emberson, J. R., Wiselka, M., Ustianowski, A., Elmahi, E., Prudon, B., Whitehouse, T., Felton, T., Williams, J., Faccenda, J., Underwood, J., Baillie, J. K., Chappell, L. C., Faust, S. N., Jaki, T., … Landray, M. J. (2020). Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19. The New England journal of medicine, 383(21), 2030–2040. https://doi.org/10.1056/NEJMoa2022926







There are lies, damn lies, and statistics, as well as, apparently, estimates. Follow the science! But wait. Now ‘science’ is a lie, too. Just ask the vaxxed and the dead.
Not your article (sorry if that’s what it sounded like)!
I’m so sick of the never-ending propaganda to kill all off-patent meds. And wow, let’s show our TDS while we’re at it!
I appreciate your patience to show how ridiculous the “analysis” really is. Most won’t wade in, which I’m sure is what they’re counting on.
5 clowns: 🤡🤡🤡🤡🤡
(My own made up rating system) 😂