Athletes, Catecholamines, and Vaccine Adverse Reactions
What factors may be responsible for the uptick in injured athletes?
Note: This is a continuation of prior Catecholamine posts. However, I decided to name this one separately. Apologies if it seems far too long and wordy! This one got away from me once again. Unfortunately, several of the citations here are derived from Cadegiani’s hypothesis as the literature is rather scant in these findings. Also, note that these articles aren’t providing a direct relationship to myocarditis or SCD, but factors that should be worth considering within the given context. Therefore, use the information below and examine them within the context of a hypercatecholaminergic state and how vaccination may work altogether to cause these issues. Please let me know if this all seems rather confusing- I can understand that!
Edit: Link included above to prior post. Apologies for not doing so before publishing this post!
Scouring the internet, and especially Substack, it’s not too difficult to come across reports about the rising cases of athletes who suffer an acute injury on the field or die suddenly mid-game. Many of these events lead to wide speculations as to what exactly is happening with these athletes and whether the vaccines are likely to play some role.
Some websites such as this one from Penny Butler1 have listed some of these deaths and injuries and appear to associate them with the vaccines, while other outlets such as Politifact attempt to “fact-check” these claims. Even as someone who tends to remain skeptical of claims without substantial evidence, it’s rather striking how Politifact can label these claims as false when they really can’t substantiate the claims (why not label it as “unsure?”, and note that Politifact relies on the use of “cause” in their argument).
Then there’s this opinion piece in Frontiers2 that provides this very interesting infograph detailing the sudden increase in reports:
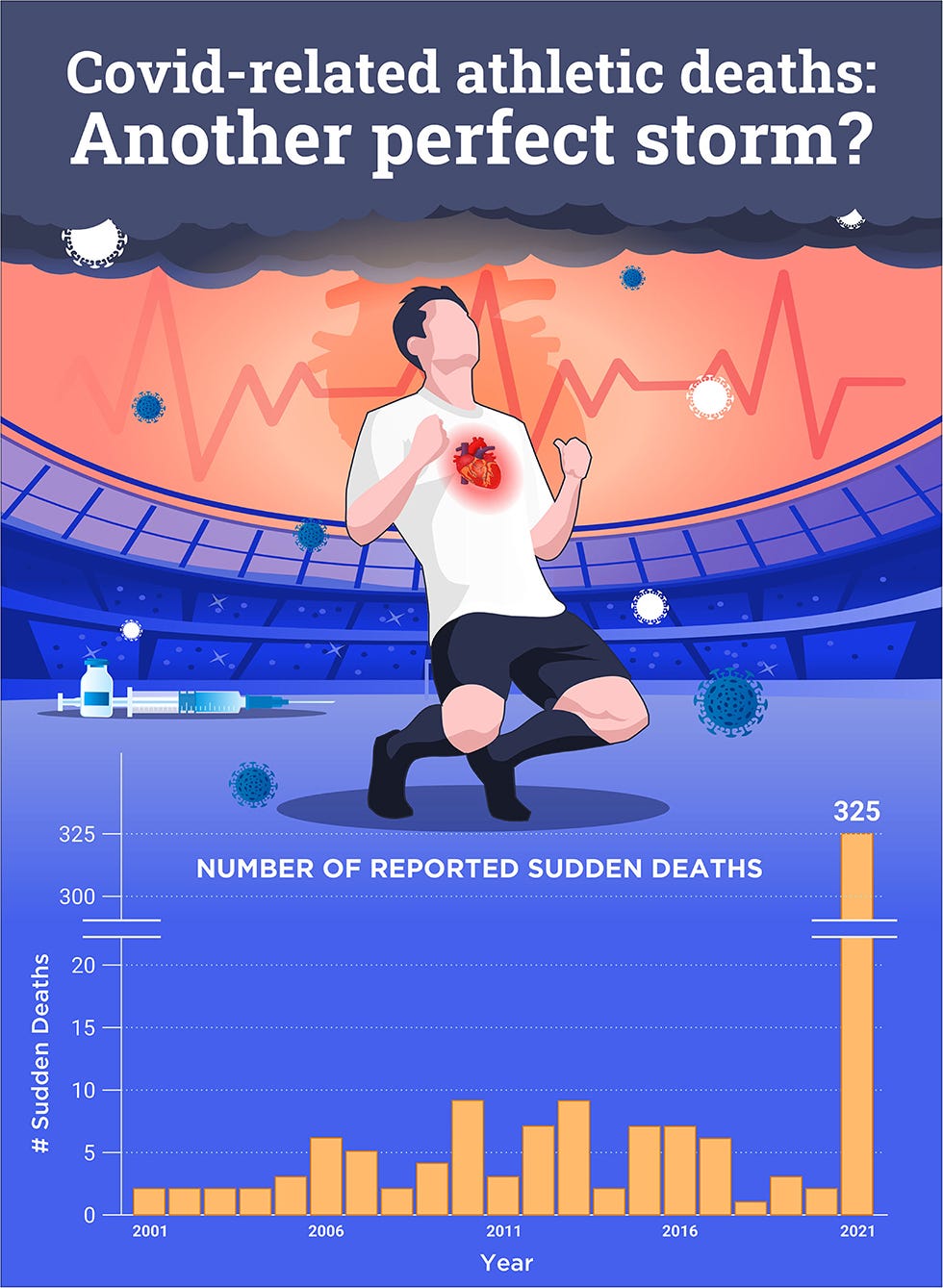
The COVID-related deaths imaged above are not specific to vaccines, but appear to insinuate both COVID infection as well as possible vaccine-related injuries as being possible drivers for this increase.
It’s quite interesting how much attention has been brought specifically to the world of athletics. Although children (in particular young men) have been the primary reference for possible vaccine-related injuries athletes are just as likely to be up there as a prime example to reference.
So why exactly are athletes being propped up in the vaccine discourse?
There’s likely several reasons for this.
Athletes are generally seen as a public figure and their ability to perform their sport puts them in the spotlight quite often. It’s hard not to obfuscate a sudden injury or death on the field when millions of people are watching.
There’s also the fact that, socially and culturally, we tend to deem athletes as the pinnacle of health and fitness. Athletes can be imagined as being the peak of human performance where only the very best within their given sport can garner acclaim and notoriety among the masses. As such, there’s a general notion that athleticism has to be correlated with some measure of health and wellness as it’s very rare to see an obese athlete.
There’s a reason why the Olympics is the grand spectacle that it is.
So in some regards there is a bit of idolatry that may influence our general perception of athletes in reference to ourselves, causing us to respond more shockingly to these injuries or deaths (remember the influence of parasocial relationships?).
Given this anecdotal evidence, and in keeping with the themes of the prior posts we’ll take a look at what role Catecholamines play in athletes and whether other factors may be worth investigating. We’ll also disabuse this association of athletes with health and explain why appearance is not a good measure of wellness.
Dr. Cadegiani’s Hypothesis on Athletes
Let’s first look back at Dr. Cadegiani’s hypothesis3 to shed some light on the route we are taking with this post. Given the current circumstances with athletes, Cadegiani outlined a few variables to see what makes athletes special given the phenomena of sudden cardiac death (SCD).
He outlines the following in his hypothesis paper (emphasis mine):
Age, sex, and athletic-level physical activity present pronounced differences in the physiology of catecholamine metabolism. Athletes, particularly male athletes, had significantly higher accumulated levels of active catecholamines, even at rest, compared to non-athletes. This observation was based on measuring 12-hour nocturnal urinary catecholamines, which refers to the accumulated release of these hormones throughout the night. While athletes had higher catecholamine levels than sex-, age-, and comorbidity-matched non-athletes, the catecholamine metabolite metanephrine remained unchanged, suggesting unaltered catecholamine clearance that led to a chronic physiological increase in exposure [41-43].
So it’s assumed that athletes, relative to the general population, may have elevated levels of Catecholamines and that much of this circulating Catecholamine may not be readily metabolized (as inferred by the “Metaneprhine unchanged” remark). As such, pairing the generally elevated levels with administration of a vaccine that itself may elevate Catecholamine levels even further may be enough to pass the threshold of minor adverse reactions to myocarditis and SCD, which Cadegiani posits in his hypothesis.
Cadegiani provides further explanation as to why athletes (in particular male athletes) may be a group of interest:
It is well-established that males present higher catecholamine responses to various stress types than females [48-50]. Moreover, both catecholamine release and beta-2 adrenergic receptor responsiveness in the cardiomyocytes are more pronounced in males than in females [51].
Although the association between sex and the age-related decrease in catecholamine activity was not reported, the age-related and sex-specific catecholamine responses and release might reflect an important interplay between catecholamines and androgens. Catecholamine responses to stress and adrenergic receptor sensitivity are enhanced in the presence of androgens [52,53]. This association with androgens is concordant with the occurrence of COVID-19 mRNA vaccine-induced myocarditis and sudden death predominantly in young males [1-5,17-20].
[…]
Myocarditis and sudden death are highly specific to young males, particularly male athletes, the population with the highest catecholamine exposure. The underlying cause of these two severe outcomes is a common hyperadrenergic state, universally demonstrated through autopsies that concluded adrenaline-induced myocarditis. Therefore, the plausibility of the hypothesis that catecholamines are the key to the occurrence of myocarditis and sudden death after COVID-19 mRNA vaccinations is considerable and is most likely but requires molecular confirmation.
To lay this route a little more clearly we’ll tackle Cadegiani’s hypothesis even further by examining 3 topics:
It’s generally assumed that Catecholamines are elevated in athletes. Therefore, evidence to support exercise as playing a role in Catecholamine elevation would be warranted to further substantiate this idea.
There appears to be an association between Androgens and Catecholamines. Although the evidence provided by Cadegiani is rather limited, we may want to investigate the literature and see what additional information there is to add.
There tends to be a very broad association between athletes and health, with the general assumption that many athletes are perfectly healthy and only dropping dead due to the vaccine. We’ll espouse on this notion and provide evidence to argue the contrary- that looks are no indication of one’s health, and in a profession mired in doing what it takes to be the best we may be inclined to argue that additional help may be afoot, and it could be this additional help that may be serving as a contraindication for cardiovascular damage.
1. Catecholamine levels among athletes
Given the fact that Catecholamines dictate many of our neuroendocrine functions and are excreted in response to stress it should come as no surprise that exercise should be associated with elevated Catecholamine levels.
Indeed, the literature of sports science appears to corroborate much of this hypothesis, with a general consensus that exercise is associated with elevated Catecholamine levels.
Take this abstract from a review article by Zouhal, et. al.4 (note this is the same researchers cited in the obesity post):
Stress hormones, adrenaline (epinephrine) and noradrenaline (norepinephrine), are responsible for many adaptations both at rest and during exercise. Since their discovery, thousands of studies have focused on these two catecholamines and their importance in many adaptive processes to different stressors such as exer-cise, hypoglycaemia, hypoxia and heat exposure, and these studies are now well acknowledged. In fact, since adrenaline and noradrenaline are the main hormones whose concentrations increase markedly during exercise, many researchers have worked on the effect of exercise on these amines and reported 1.5 to >20 times basal concentrations depending on exercise characteristics (e.g. duration and intensity). Similarly, several studies have shown that adrenaline and noradrenaline are involved in cardiovascular and respiratory adjustments and in substrate mobilization and utilization.
The review is rather interesting and takes a look at gender differences and differences in sports and their effects on Catecholamines, so it may be worth a read for additional context. In the meantime I’ll note a few studies that I came across to corroborate this consensus.
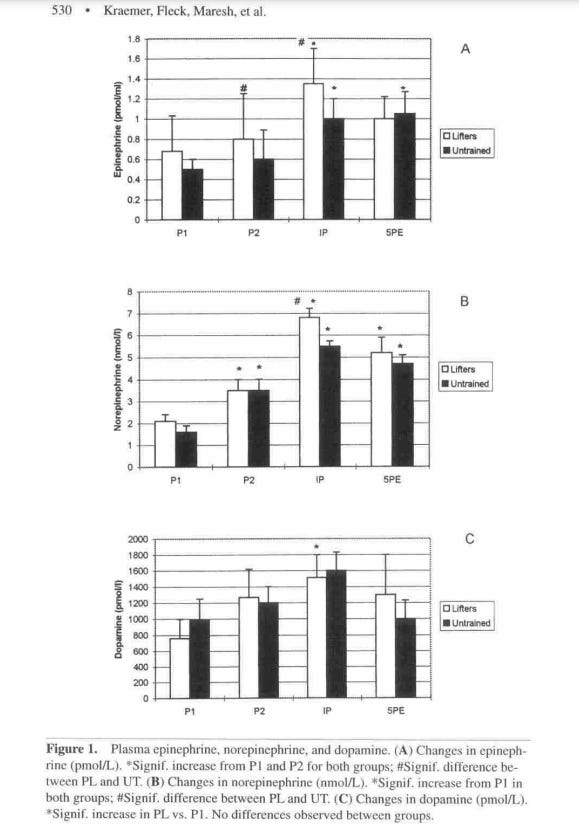
In one study by Kraemer, et. al.5 researchers looked at the levels of Catecholamine released after exercise among power lifters and compared them to untrained individuals. Seven male powerlifters and 12 untrained men were tasked with engaging in bilateral leg presses and had blood samples drawn at various time points and measured for Catecholamines. Blood samples were drawn twice pre-exercise (labeled P1 and P2, respectively), once immediately after exercise (PI), and 5 minutes post-exercise (5PE), with the results showing that post-exercise Catecholamine levels were higher than pre-exercise levels. Also, powerlifters tended to show elevated levels of Norepinephrine and Dopamine compared to untrained individuals:
One interesting study by Nagao, et. al.6 looked at the association between Catecholamine levels and the migration of natural killer (NK) cells during exercise, with findings suggesting that Catecholamines reduce the expression of adhesion molecules on the surface of NK cells allowing them to migrate into the bloodstream.
In this study 8 non-smoking males were tasked with exercising on an ergonomic bike for 30 minutes, and blood samples were taken 10 min before exercise, immediately after exercise, and at intervals of 5, 15, 30, and 60 min post-exercise.
The work in this study focused on the premise that elevated Catecholamine levels were found during exercise, and that migration of innate immune cells (likely from germinal centers to the extremities of the body) is also generally noticed. Pairing the two together provides for some possible biochemical association, and it appears that activation of adrenergic receptors on the surface of NK cells may reduce the presence of CD44 adhesion molecules as corroborated by a mouse experiment in which mice were given exogenous Norepinephrine:
In this study, we demonstrated that the dynamic change in peripheral blood NK activity during and after an exercise is associated with mobilization of NK cells, which appears to result from modulation of adhesion molecules such as CD44 on NK cells by exercise-induced catecholamines. In support of this notion, an intravenous injection of norepinephrine into mice induced a rapid mobilization of NK cells into circulation in association with downmodulation of adhesion molecules on NK cells.
These findings are very interesting as it corroborates some of the arguments in regards to an “open-window” hypothesis with exercise, such that exercise may lead to migration of innate immune cells and suppress immune function post-exercise, especially after arduous training regimens.
I discuss this hypothesis in one of my exercise posts, and although such a hypothesis is quite controversial it’s interesting to see that there could be an association between Catecholamines and possible overtraining.
Expanding even further, a great deal of Cadegiani’s work rests within the field of sports science and overtraining; three of the above citations listed in his hypothesis are actually derived from his prior work (Citations 41-43).
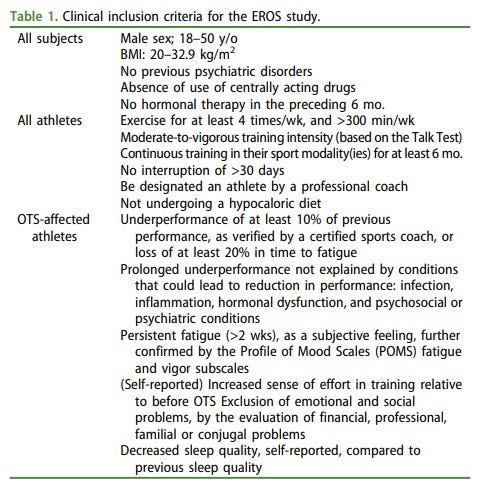
For instance, one of his pivotal works was the EROS study7. EROS stands for the Endocrine and Metabolic Responses on Overtraining Syndrome. It’s a bit of a mouthful, but in this post-hoc study, which utilized findings and measures from various portions of the EROS study, Cadegiani, et. al. looked at biomarkers for people who show symptoms of overtraining (OTS- overtraining syndrome) and compared them to “healthy” athletes (ATL) and non-physically active controls (NPAC).
OTS is a rather subjective phenomenon, but it is generally defined as:
an imbalance between training load, rest and nutrition that results in chronic fatigue and reduced performance (definition modified from Cadegiani, et. al.).
Why exactly the body undergoes OTS is an interesting matter. General hypotheses suggest that this is the body’s way to compensate for the demands of continuous training by providing the body with the proper neuroendocrine signaling molecules to keep going and moving, although at the consequence of other biochemical processes such as the dampening of the immune system and other biological functions that act antagonistically to the sympathetic nervous system (such as digestion).
The focus of this EROS study was to examine the effects that high-intensity functional training (HIFT- or CrossFit as it’s most well-known example) had on biomarkers. CrossFit athletes were categorized based on criteria that matched either OTS or ATL. Participants were also included who had no indication of exercise in the 3 years prior (the NPAC group). In the end 9 OTS participants, 22 ATL participants, and 12 NPAC were included and had measures of biochemical molecules and hormones collected either through specific hormone tests or through night-time urinary samples.
Of interest is the basal measures (biochemical and hormonal measurements at rest) of these participants, which indicate that measures of Catecholamines were significantly higher among athletes who experienced OTS compared to ATL athletes and NPAC participants while not physically active:
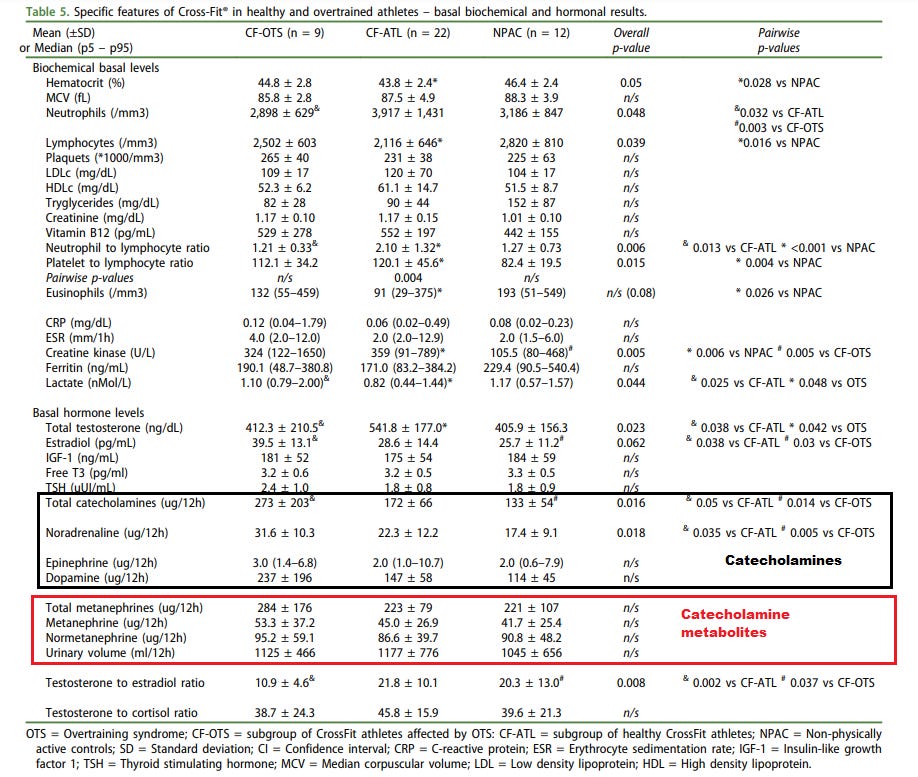
As can be seen most measures of Catecholamines were elevated even at rest for OTS athletes (273 vs 172 and 133 ug/12h, respectively), and it appears that the level of Metanephrines8 (Catecholamine metabolites) did not statistically differ compared to ATL and NPAC individuals.
There are a few limitations for this study, as the categorization of OTS can be considered highly subjective and can be based on multiple self-reported factors9. This may bias the categorization of OTS as several factors may be responsible for the presentation of OTS. This is generally corrected for with the ATL and the NPAC groups, and Cadegiani suggests in his Cureus bio that his work uses a rather robust criteria to categorize OTS.
Also, although some of these measures showed statistical significance (such as the total Catecholamine and Noradrenaline levels among OTS athletes compared to the other athletes) the Metanephrine group didn’t appear to reach statistical significance even though the range for these measures vary greatly. Cadegiani mentions in his hypothesis article that these levels remained unchanged, and I would actually argue that may be a mischaracterization of the measured levels (a range of 176 ug/12h is a very wide range, especially compared to the ATL and NPAC group).
This may be a consequence of uneven sampling and low numbers in general which is a general issue in sports science studies. The Kraemer, et. al. and Nagao, et. al. study cited above certainly have low numbers of participants. They both also differ in their exercise regimens (former weight training; latter cardio), and both differ in how Catecholamine measures were taken (Cadegiani, et. al. measured nightime urinary Catecholamine levels whereas the other two measured plasma levels) and may be factor in heterogeneity of the data.
So overall how do these studies relate to the case of athletes and the increase in injuries?
Well, we may be able to assume that athletes will have a higher level of Catecholamines during exercise-this seems to be evident within the literature, although it appears that different exercises/regimens may lead to different levels of Catecholamines released (apparently the Catecholamine levels measured by Cadegiani, et. al. among CF athletes are higher than is traditionally found in other sports, possibly due to the combination of functional training exercises exerting different stresses on the body).
If we take the scenario of a post-vaccinated athlete the stress on the body due to training or a game immediately after vaccination may push the risk of adverse reactions past the threshold into possible cardiac damage or SCD. In combination with the fact that different sports may result in different levels of elevated Catecholamines, it may be worth investigating which sports may be at increased risk due to Catecholamine levels.
This can actually be seen in a study by Batatinha, et. al.10 in which athletes were asked to participate in a graded exercise weeks post-vaccination. Participants either received 2-doses of Pfizer’s COVID vaccine or one dose of J&J’s, and biochemical/physiological measures were taken to see whether vaccination would alter physiological performance.
Overall, it appears that performance was not affected when compared between vaccinated and unvaccinated athletes. However, vaccinated athletes showed elevated heart rates and higher levels of Norepinephrine.
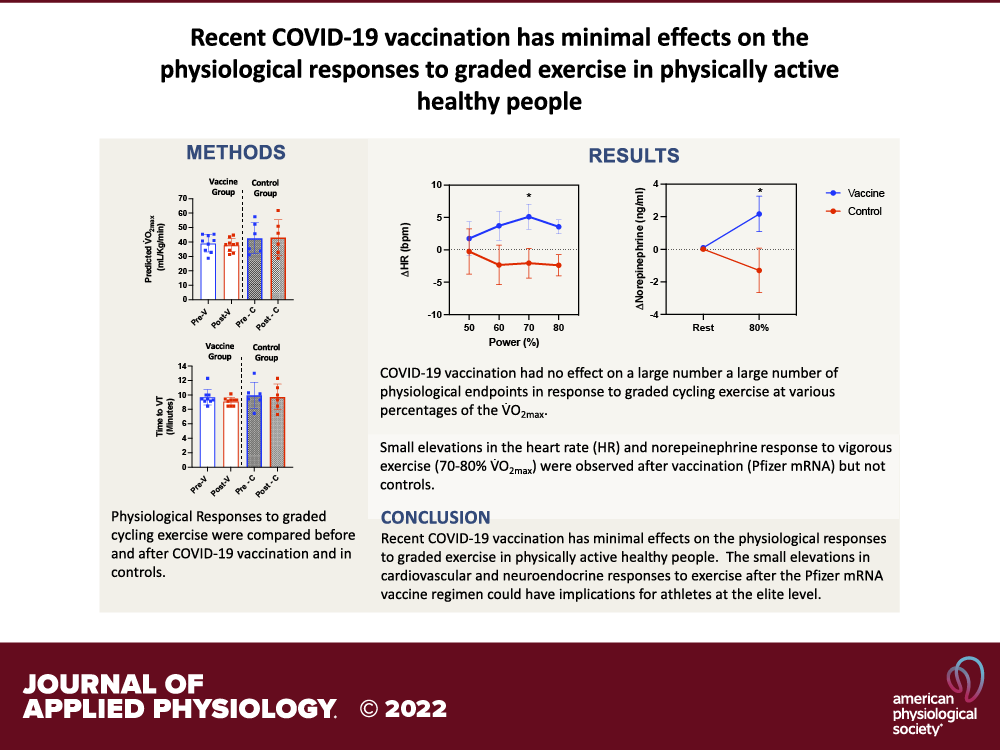
What’s interesting about this study is that it took measures from athletes before vaccination, which actually provided a baseline for these individuals (the study was separated into 3 visits with Visit 1 being pre-vaccination and Visits 2/3 occurring 1-3 weeks post-vaccination). When stratified between pre/post vaccination it appears that Norepinephrine levels were significantly elevated post-vaccination when exercising at 80% maximum oxygen volume, suggesting a possible elevated Catecholamine level associated with vaccination.
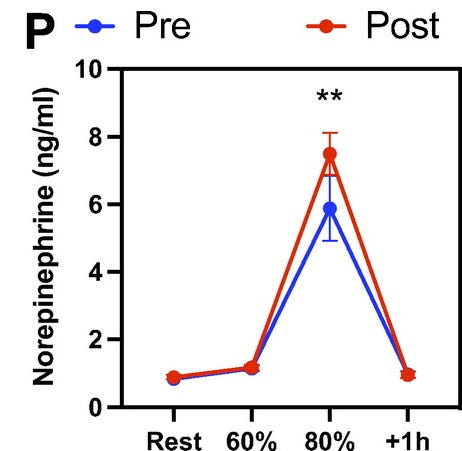
The researchers provide this remark in regards to these findings:
We did, however, find significant elevations in heart rate (∼5 beats/min) and norepinephrine responses to vigorous (e.g., 70%–80% V̇O2max) intensity exercise after vaccination, particularly in those who received the two-dose Pfizer mRNA vaccine regimen. Neither heart rate nor norepinephrine changed in demographically matched control participants who completed identical bouts of exercise several weeks apart without receiving a vaccine. Although it is possible that these effects are due to reduced physical activity levels after vaccination (e.g., due to symptoms of vaccinosis), we deem a detraining effect unlikely as, despite reporting many of the common symptoms associated with COVID-19 vaccination, our participants did not report significant changes to their physical activity levels during the study period. The mechanisms by which recent COVID-19 vaccination might increase cardiovascular responses to graded exercise in healthy people are not known, although the elevated heart response after vaccination may have been driven by the concomitant elevation in the norepinephrine response to exercise (20). A more detailed examination of the cardiovascular and neuroendocrine responses to graded exercise after COVID-19 vaccination would be illuminating.
This is one of the only studies detailing an actual elevation of Catecholamines post-vaccination, and provides evidence that a hypercatecholaminergic state may be associated with vaccination and exercise via having a synergistic effect, although it’s worth noting that these tests were conducted 1-3 weeks post-vaccination and may not be an accurate measure of Catecholamine levels days after vaccination.
That leaves us with the matter of OTS, which is rather difficult to associate directly with athletes. As Cadegiani outlined in his work overtraining appears to lead to the greatest levels of Catecholamines released when compared to “healthy” athletes or untrained individuals.
To what extent most professional athletes would fall under this category would be one of speculation, as there is no quantifiable measure of OTS among athletes, or if they would be aided by other methods to reduce fatigue and other symptoms of OTS.
It may be assumed that at the professional level such extreme exertion may be necessary that OTS is likely a common phenomenon, but once again the literature is quite conflicted due to the high degree of subjectivity in defining and quantifying OTS.
One thing that seems to be made clear about OTS is that there is a large mental health factor in OTS, as mental stress may also exacerbate the effects of OTS by causing chronic stress and continuous circulation of elevated Catecholamine levels, meaning that there may be far more than just physical exertion at play here.
In short, it’s clear that exercise leads to elevated Catecholamines, and there appears to be some evidence that this elevation is even higher post-vaccination and may be associated with some synergistic effect due to exercise. As the entire sports profession revolves around continuous, arduous exercise we may posit that Catecholamine levels may be fairly elevated in comparison to the general population. The combination of these Catecholamine-elevating factors may be enough to cause the myocarditis and SCD seen in these athletes and young men, and it may explain why many of these injuries occur during an actual game when both stress and physical exertion is likely to be at very high levels.
However, given the multitude of circumstances for athletes there are also many underlying factors that should be considered, and it’s like that the accumulation of other extraneous factors may be contributing to this phenomenon and should warrant additional, contextual investigations.
2. The relationship between Catecholamines and Androgens
The association proposed by Cadegiani between Catecholamines and Androgens is not one specific to athletes, but given the current concerns over young males we may want to see if Catecholamines and Androgens may share some biochemical relationship.
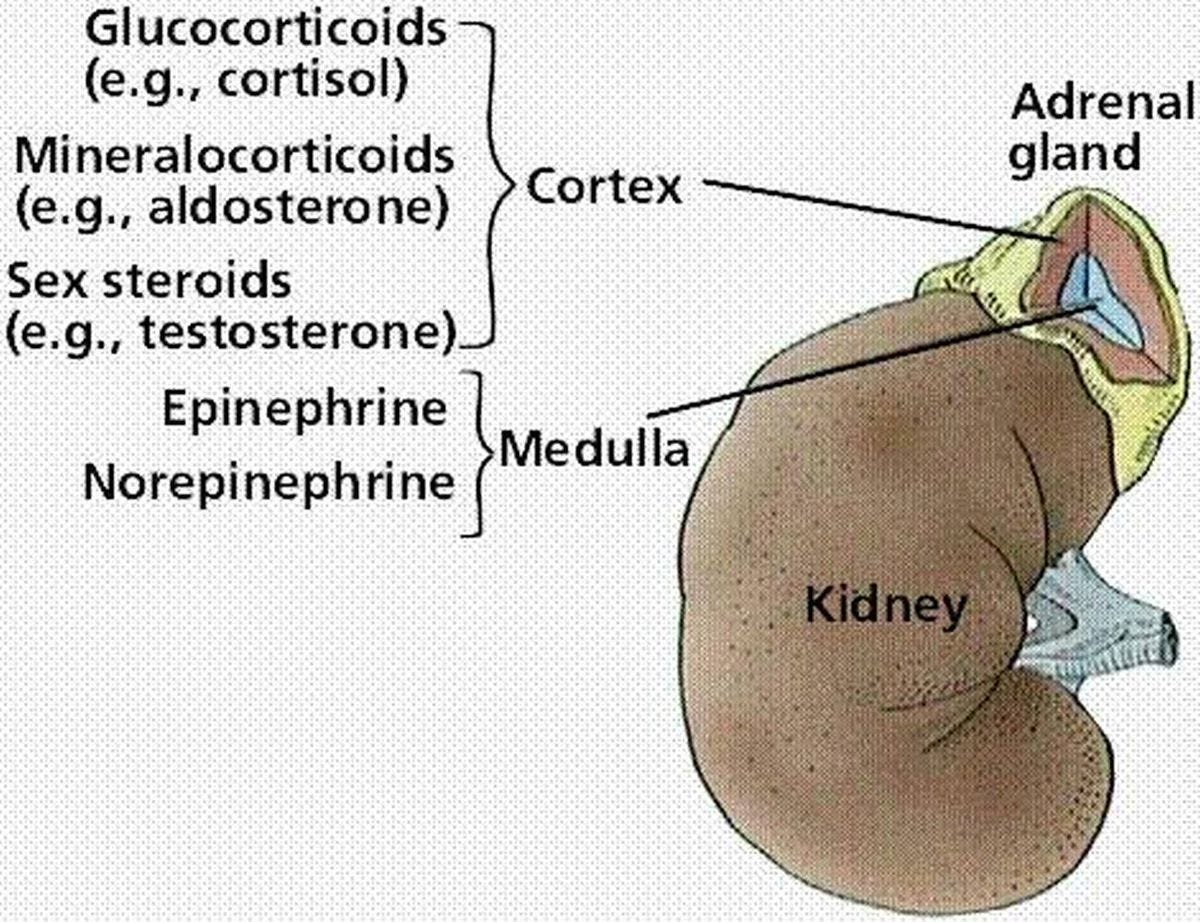
If we look at the anatomy of the adrenal gland we can see that the proximity of the medulla to the cortex (both being part of the adrenal gland) may reveal some evolutionary relationship, such that these biochemical compounds may upregulate/downregulate one another.
What’s interesting is that the association between Catecholamines and Androgens such as Testosterone may be found by looking at fat metabolism. As we detailed in the prior post lipolysis depends on the expression of adrenergic receptors, and it appears that Testosterone may be responsible for upregulation of some of these adrenergic receptors (Lee, et. al.11, [context included]):
The receptors for androgen are present in adipose tissue, and are more prominent in visceral (VAT) than subcutaneous adipose tissue (SCAT).40 Among various hormones that regulate the metabolism of adipocytes, catecholamine plays an important role in controlling lipolysis and receptors for catecholamines, known as adrenoreceptors [same as adrenergic receptors], increase in density by testosterone. Testosterone also influences adipose tissue by up-regulating the adrenoreceptor (AR) that activates lipolysis.41 An experiment on adipose precursor cells of male rats suggested that testosterone stimulated catecholamine-induced lipolysis in a dose-dependent manner through β-AR [adrenergic receptor] and adenylate cyclase.42 In particular, lipolysis induced by testosterone was consistently observed, even after treatment with ARO [aromatase → enzyme that converts testosterone into estrogen] inhibitor, proving that the effect was not due to the estrogens converted by ARO.42
This suggestion is very revealing for the fact that Testosterone has been inversely proportional to obesity, such that lower Testosterone levels in men have been associated with higher body fat and reduced lean mass12. This may indicate an intrinsic function of Testosterone in which elevated levels of Testosterone may upregulate the response to Catecholamines and increase lipolysis within adipocytes. The reference to adipocytes is what's important here, as we'll explain that the interplay between Testosterone and Catecholamines is wholly dependent on the cell and organ being targeted.
It’s worth noting that, when examining the Cadegiani, et. al. chart from the EROS study Testosterone levels appear to take on a normal curve (peak in the middle for ATL with dips on both ends for NPAC and OTS) whereas Catecholamine levels take on a J-curve from NPAC → ATL → OTS. Such a finding may indicate that Catecholamines and Testosterone may be released as a result of exercise to influence signaling and biological processes, but continuously elevated levels of Catecholamines through overtraining may be associated with a deleterious effect in which Testosterone production may be attenuate or reserves may be depleted.
Overall, the relationship between Testosterone and Catecholamines is rather nuanced and complex.
Testosterone’s effects on the body are organ-specific and may be mediated either through genomic or non-genomic effects. This would make sense given Testosterone’s role as an endocrine hormone.
Essentially, genomic effects are ones in which Testosterone upregulates the transcription and expression of various genes usually through binding of Testosterone to androgen receptors (AR) while non-genomic effects are direct agonist/antagonistic effects of Testosterone on cellular enzymes and receptors.
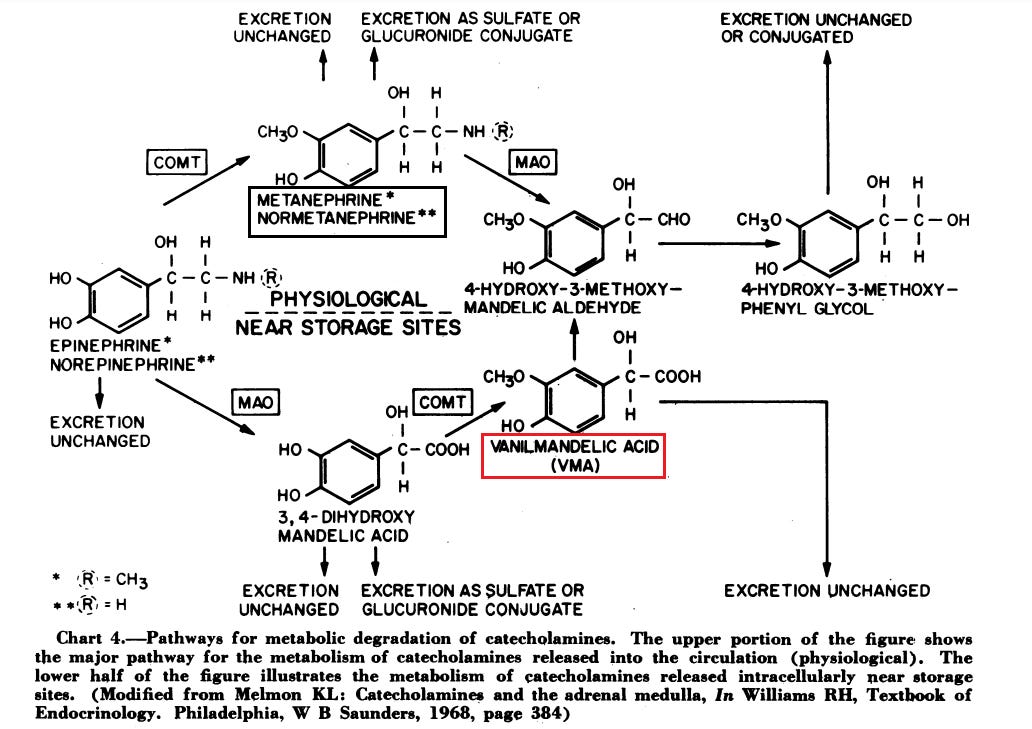
For instance, Testosterone’s effects on the expression of β-AR would be a genomic effect whereas Testosterone’s inhibitory effects on enzymes such as catechol-O-methyl transferase (COMT) may be considered nongenomic.
This nuanced examination can be seen in one review by Carbajal-García, et. al.13 which reviews the genomic and nongenomic effects of Testosterone on adrenergic responses in various muscles and tissues such as the heart and lungs.
The review is rather dense, but some of the information can be summarized within the conclusion:
The adrenergic system plays a pivotal role in the control of vascular, airway, and cardiac physiology. A relationship between androgens with the adrenergic system of these tissues is proposed. This review summarizes that, in the vascular smooth muscle, T [testosterone], via the androgen receptor, reduces the AC [adenylyl cyclase → enzyme that converts ATP into cyclic AMP] expression and increases the α1-AR expression, leading to high BP [blood pressure] and hypertension. Moreover, in the airway smooth muscle, T, via nongenomic action, potentiates the β-adrenergic-induced relaxation through the inhibition of COMT [catechol-O-methyl transferase → converts Catecholamines into Metanephrine (refer to Footnote 6 for a diagram)] or by the abolition of extraneuronal uptake. This androgen, via a genomic effect, also augments the expression of β2-AR and induces an increase in the relaxing responses to salbutamol. In the cardiac muscle, T upregulates the expression of α1A-AR and β2-AR mediated by the AR signaling, improving the myocardial performance. Moreover, T also increments β1-AR expression, improving the cardiomyocytes’ function; however, the enhancement in muscle work during a long period ends up developing hypertrophy and heart failure.
There’s a lot to take in here, but the general premise is that Testosterone has different effects on Catecholamines depending on the organ and the type of effect (genomic vs nongenomic) that Testosterone has on cells. As such, it’s rather difficult to look at studies comparing androgen function and fully elucidate the processes that are at play.
One factor that may be worth examining is puberty and possible associations between androgen release and Catecholamines. It’s generally assumed that puberty is met with a rampant increase in androgens that aid in maturation and growth, but how this relates to Catecholamines is another matter.
Although this relationship itself is confusing with no clear association, there is one group that provides some interesting information, and that’s children who undergo precocious puberty.
Precocious puberty is early onset puberty usually marked by sexual maturation and behavioral changes earlier than should be expected. Apparently the rate of precocious puberty is on the rise, and this phenomenon appears to occur in young girls more often than boys.
The causes of precocious puberty vary, with some remarking that a combination of genetic and environmental factors may be responsible.
As to this article, it’s the environmental factors that are worth examining.
For instance, a case report from Ergür, et. al.14 looked at Methylphenidate (Ritalin) use in children with ADHD and the diagnosis of precocious puberty- remember that stimulants such as Adderall and Ritalin inhibit the reuptake of Dopamine and Norepinephrine while also inhibiting the enzyme MOA that metabolizes these Catecholamines.
This was a very small case report of only 7 children (4 girls, 3 boys) who were on Ritalin for about 6 months and showed evidence of precocious puberty. There is no direct association between stimulants and precocious puberty (aside from tests of LH-releasing hormone which show pubertal growth), so this information should be taken with skepticism.
More important than this finding may be the hypothesis laid out by the researchers:
PPD [precocious puberty] is a consequence of decreased activity of central suppressor system on GnRH [gonadotropin-releasing hormone → controls release of luteinizing hormone and follicle-stimulating hormone which aid in puberty] neurons and the increased activity of the prominence excitatory systems. Glutamine, dopamine, and noradrenaline are the most important excitatory neurotransmitters that have a role in starting puberty.11) The effect of MPH [Methylphenidate i.e. Ritalin], cumulating dopamine and noradrenaline in the synaptic gap, may induce puberty by affecting their own receptors. There are some animal study evidences that confirm this hypothesis; in the study of Adriani et al.,12) 2 mg/kg/day MPH and saline have been injected on 30 to 44 days old rats. They observed that in the MPH injected group, weight of testicles and amount of sperm have increased and these findings interpreted as subchronic MPH exposure in adolescent rats could have a trophic action on testis growth and a negative impact on testosterone metabolism.
[…]
As conclusion, using psychostimulant drugs at childhood may accelerate puberty with the excitatory effect of dopamine’s and noradrenaline’s GnRH release and with the disappearance of GnRH receptor expression suppressor effect on prolactin’s HPGA [hypothalamic-pituitary-gonadal axis → the relationship between the brain, pituitary gland, and the gonads] region with prolactin disinhibitory effect. In this case series, the story of PPD in MPH treated children with high/normal BMI is quite remarkable.
I came across this study as it was part of a review examining the increased levels of precocious puberty in Italian girls over the course of the lockdowns.
The reviewers Street, et. al.15 describe how diagnoses of precocious puberty appear to be on the rise among young girls since the start of the lockdowns. They hypothesize that several environmental factors such as viral infection, stress due to lockdowns and social isolation, as well as increased exposure to endocrine disruptors from staying indoors (all consequences of lockdowns) all may contribute to increasing precocious puberty rates.
The Catecholamine idea is one of interest here, and although it draws from limited data it does propose something worth investigating:
Psychologists have correctly defined the pandemic as “a biological disaster with a subsequent strong psychological impact” (13). Increased catecholamines (dopamine and norepinephrine-NE) can also accelerate puberty; this has been shown in a female mouse model where both basal and potassium stimulated NE, after treatment with a partially purified male urine extract, was found to be increased in the posterior part of the olfactory bulb (14). Moreover, one study, in humans, reported increased precocious puberty after the use of methylphenidate, currently used for the treatment of attention deficit hyperactivity disorder, which blocks dopamine and NE transporters increasing their concentration in synaptic gaps (15)[study I cited above]. These could be capable of triggering puberty, and although these data still need to be confirmed, they might represent indirect evidence of a possible effect of catecholamines that needs to be further studied. It is currently unknown how much these mechanisms could be really of importance in humans.
How precocious puberty relates to regular puberty is an important question, as the pathways for precocious puberty may not be as simple as regular puberty but occurring earlier via early release of hormones. This means that this may not tell us exactly whether Catecholamine release is vital to regular puberty and may play a role in the elevated myocarditis risk in teenage boys.
Nonetheless, this provides for an initial point which may be worth investigating to see what specific role Catecholamines may play in puberty.
Overall, what can we gather in regards to Androgens and Catecholamines?
The relationship between Androgens and Catecholamines is extremely nuanced. There’s no immediate association between the two that can be used to argue the myocarditis risk, although we can see that Testosterone can have widespread effects on different organs of the body and alter responses to Catecholamines. Interestingly, elevated Testosterone has been associated with high blood pressure and possible cardiovascular disease, which may raise questions as to whether elevated levels of Testosterone may have deleterious effects that compound with the concerns over a hypercatecholaminergic state.
However, the results from Cadegiani, et. al. and other researchers indicate that regular athletic training may elevate Testosterone levels while overtraining may reduce these levels. At the same time, overtraining appears to be associated with elevated Catecholamines overall, meaning that multiple other factors are responsible for elevated Catecholamine levels independent of Testosterone.
The possible links between Catecholamines and precocious puberty warrant additional investigation to examine whether these initial reports provide insight into the role Catecholamines play in puberty. Considering that young men are likely to be undergoing puberty it may be of importance to see whether puberty is associated with some type of hyperadrenergic response.
It’s worth noting that Testosterone can have deleterious effects on the body, and therefore when examining these athletes one may wonder whether hormonal alterations via exogenous substances may factor into the rates of SCD seen. Once again, it’s the accumulation of factors that must be examined.
It’s for this fact, and the fact that these SCD cases are occurring in athletes that we may want to examine other extraneous factors that are necessary for this discussion. Remember that athletes must be at the top of their profession, inclining athletes to “do whatever it takes”, and it may be for this fact that athletes may put themselves at risk of adverse reactions. We’ll describe some of these issues in more detail in the next post.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

Note that I am unaware of who Penny Butler is and am linking this website merely as an example of collected athlete information.
Maffetone, P. B., & Laursen, P. B. (2022). COVID-Related Athletic Deaths: Another Perfect Storm?. Frontiers in sports and active living, 4, 829093. https://doi.org/10.3389/fspor.2022.829093
Cadegiani F A (August 11, 2022) Catecholamines Are the Key Trigger of COVID-19 mRNA Vaccine-Induced Myocarditis: A Compelling Hypothesis Supported by Epidemiological, Anatomopathological, Molecular, and Physiological Findings. Cureus 14(8): e27883. doi:10.7759/cureus.27883
Zouhal, H., Jacob, C., Delamarche, P., & Gratas-Delamarche, A. (2008). Catecholamines and the effects of exercise, training and gender. Sports medicine (Auckland, N.Z.), 38(5), 401–423. https://doi.org/10.2165/00007256-200838050-00004
Kraemer, William & Fleck, Steven & Maresh, Carl & Ratamess, Nicholas & Gordon, Scott & Goetz, Kenneth & Harman, Everett & Frykman, Peter & Volek, Jeff & Mazzetti, Scott & Fry, Andrew & Marchitelli, Louis & Patton, John. (2000). Acute Hormonal Responses to a Single Bout of Heavy Resistance Exercise in Trained Power Lifters and Untrained Men. Canadian journal of applied physiology = Revue canadienne de physiologie appliquée. 24. 524-37. 10.1139/h99-034.
Fumiko Nagao, Masatoshi Suzui, Kazuyoshi Takeda, Hideo Yagita, and Ko Okumura
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology2000279:4,R1251-R1256
Cadegiani, F. A., Kater, C. E., & Gazola, M. (2019). Clinical and biochemical characteristics of high-intensity functional training (HIFT) and overtraining syndrome: findings from the EROS study (The EROS-HIFT). Journal of sports sciences, 37(11), 1296–1307. https://doi.org/10.1080/02640414.2018.1555912
Helena Batatinha, Forrest L. Baker, Kyle A. Smith, Tiffany M. Zúñiga, Charles R. Pedlar, Shane C. Burgess, Emmanuel Katsanis, and Richard J. Simpson
Journal of Applied Physiology2022132:2,275-282
Lee, H. K., Lee, J. K., & Cho, B. (2013). The role of androgen in the adipose tissue of males. The world journal of men's health, 31(2), 136–140. https://doi.org/10.5534/wjmh.2013.31.2.136
Kelly, D. M., & Jones, T. H. (2015). Testosterone and obesity. Obesity reviews : an official journal of the International Association for the Study of Obesity, 16(7), 581–606. https://doi.org/10.1111/obr.12282
Abril Carbajal-García, Jorge Reyes-García, Luis M. Montaño, "Androgen Effects on the Adrenergic System of the Vascular, Airway, and Cardiac Myocytes and Their Relevance in Pathological Processes", International Journal of Endocrinology, vol. 2020, Article ID 8849641, 25 pages, 2020. https://doi.org/10.1155/2020/8849641
Ergür, A. T., Gül, H., & Gül, A. (2019). Methylphenidate and Central Precocious Puberty: A Probable Side Effect among Seven Children with the Attention Deficit Hyperactivity Disorder. Clinical psychopharmacology and neuroscience : the official scientific journal of the Korean College of Neuropsychopharmacology, 17(3), 446–449. https://doi.org/10.9758/cpn.2019.17.3.446
Street, M. E., Sartori, C., Catellani, C., & Righi, B. (2021). Precocious Puberty and Covid-19 Into Perspective: Potential Increased Frequency, Possible Causes, and a Potential Emergency to Be Addressed. Frontiers in pediatrics, 9, 734899. https://doi.org/10.3389/fped.2021.734899


4 thumbs up! Lots to digest. Mahalo for the research.
excerpt-"One thing that seems to be made clear about OTS is that there is a large mental health factor in OTS, as mental stress may also exacerbate the effects of OTS by causing chronic stress and continuous circulation of elevated Catecholamine levels, meaning that there may be far more than just physical exertion at play here."
Exactly... the fight or flight response is activated by the person.. meaning.. they assume the "beast mentality" to get their bodies going in order to get to muscle failure.