And now suicidal ideation?
European and UK agencies are looking into signals of suicidal ideation and self-harm after use of GLP-1 receptor agonists such as Ozempic or Wegovy.
As more people hop onto the GLP-1 RA bandwagon with drugs such as Wegovy or Ozempic more reports of concerning safety issues are making their way into the media, with the next big concern being possible suicidal ideation and self-harm in those taking these drugs.
So far, the reports provided are anecdotal and relegated to adverse events reporting systems. Nonetheless, the signal appears to be enough that several agencies are looking into these reported safety signals.
For instance, the European Medicines Agency listed both Liraglutide (sold as Victoza and Saxenda) and Semaglutide (Wegovy/Ozempic) as a topic of discussion for their July pharmacovigilance agenda:
As the EMA reports in a November article, the emerging safety signal was brought on by initial reports to Iceland’s medicine agency, which eventually led to over 150 documented reports by the EMA:
EMA’s safety committee, the PRAC, is reviewing data on the risk of suicidal thoughts and thoughts of self-harm with medicines known as GLP-1 receptor agonists,1 including Ozempic (semaglutide), Saxenda (liraglutide) and Wegovy (semaglutide). These medicines are used for weight loss and for treating type 2 diabetes.
The review was triggered by the Icelandic medicines agency following reports of suicidal thoughts and self-injury in people using liraglutide and semaglutide medicines. So far authorities have retrieved and are analysing about 150 reports of possible cases of self-injury and suicidal thoughts.
Liraglutide and semaglutide medicines are widely used, with an exposure of over 20 million patient- years2 to date. It is not yet clear whether the reported cases are linked to the medicines themselves or to the patients’ underlying conditions or other factors.
Note that there’s a strong relationship between obesity, diabetes, and depressive symptoms, and so one has to consider the fact that underlying suicidal thoughts may be derived from factors that would lead one to seek out these GLP-1 RA medications, and may not be directly related to the actual drug.
The EMA is expected to provide a report this month in regards to their investigation.
In the meantime, the question remains why suicidal ideation would even be a factor in a possible weight-loss medication.
As several readers have mentioned, one clear thing worth considering is the fact that these GLP-1 RAs are not just typical, one-action drugs, but rather are acting as hormone mimetics for native GLP-1.
As GLP-1 shows widespread effects on the body it may not come as a surprise that a drug that not only binds to GLP-1 receptors, but does so more strongly with reduced metabolism relative to native GLP-1, may also elicit other unwanted effects.
This can be seen in reports of stomach paralysis in some individuals taking these drugs, which may suggest an overexaggerated response otherwise not produced by native GLP-1:
Users of Ozempic-like drugs report stomach paralysis as a side effect
Apologies for readers who may find these reports on Ozempic and other GLP-1 receptor agonists a bit tiring. I personally find that there’s a lot to glean from this Ozempic…
Which is further corroborated by the FDA including intestinal paralysis on Ozempic’s label:
FDA updates Ozempic label to include intestinal paralysis as an adverse reaction
On September 22nd the FDA added an additional warning to Ozempic’s label, this time noting ileus, or intestinal paralysis, as a post-marketing adverse reaction, suggesting that these adverse reaction…
And due to the fact that Ozempic-like drugs are being examined for their possible role in helping treat addiction:
Will Ozempic be used to treat addiction?
Modern Discontent is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber. Now that GLP-1 receptor agonists such as Ozempic have seen g…
Indeed, it does appear that there may be a relationship between GLP-1 and depression, which has led researchers to wonder if GLP-1 RAs may aid in treating depressive symptoms.
A review from Detka, J., & Głombik, K.1 notes some of these possibilities, which includes reduction of neuroinflammation, restoration of the gut-brain axis, and other benefits that may come from GLP-1 RAs:
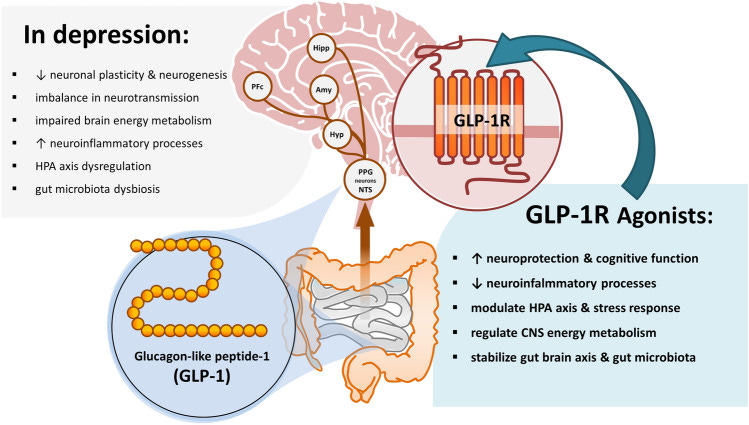
Again, keep in mind that obesity, poor diet, and microbiome dysfunction may play causative roles in depression, and so it’s quite possible that GLP-1 RAs may help to restore homeostasis that may have been lost.
Another review from Laurindo, et al.2 notes that GLP-1 RAs may help to improve neurogenesis (production of neurons) and production of neurotransmitters:
The neurotransmitter imbalance (serotonergic, dopaminergic, and noradrenergic dysfunctions) is directly related to neuroinflammation and can lead to behavioral changes and behavioral impairment. The stimulation of GLP-1 receptors in the cerebral cortex and hippocampus is related to the modulation of serotonin, dopamine, gamma-aminobutyric acid, and glutamate. Additionally, GLP-1 stimulates dopamine turnover in the amygdala due to its actions on dopamine receptor 2. Due to these effects as a neurotransmitter release supporter, GLP-1 can be related to the amelioration of depressive behavioral signals and symptoms [84,85,88].
Depression is related to impairments due to neurogenesis, principally in the hippocampus, as well as neuronal atrophy and a decreased volume of several neuronal areas, such as the hippocampus, cortex, and limbic lobe regions of the brain. These regions are related to emotion and cognition in the normal brain. Decreased hippocampus volume and hippocampus atrophy are related to depressive episodes in patients affected by depression. Past studies demonstrated that the stimulation of neurogenesis in the hippocampus influences emotional regulation and depression, acting as an anti-depressant molecule due to increased serotonin receptors’ increased activity and reduced neuronal loss by neuronal replacement. GLP-1 can stimulate neurogenesis by several different pathways. Studies with human neuronal cells could demonstrate that GLP-1 increases cell proliferation, and studies with animal models could indicate the stimulation of the neuronal cells by GLP-1 and by the activation of GLP-1 receptors. In rodent models, liraglutide promoted neurogenesis in the hippocampus. In mouse models, neurogenesis was activated by the GLP-1 stimulations of cAMP/PKA and Akt/GSK3 cellular signaling pathways [84,85,88]. Figure 9 shows some effects of GLP-1 in the pathophysiology of depression.
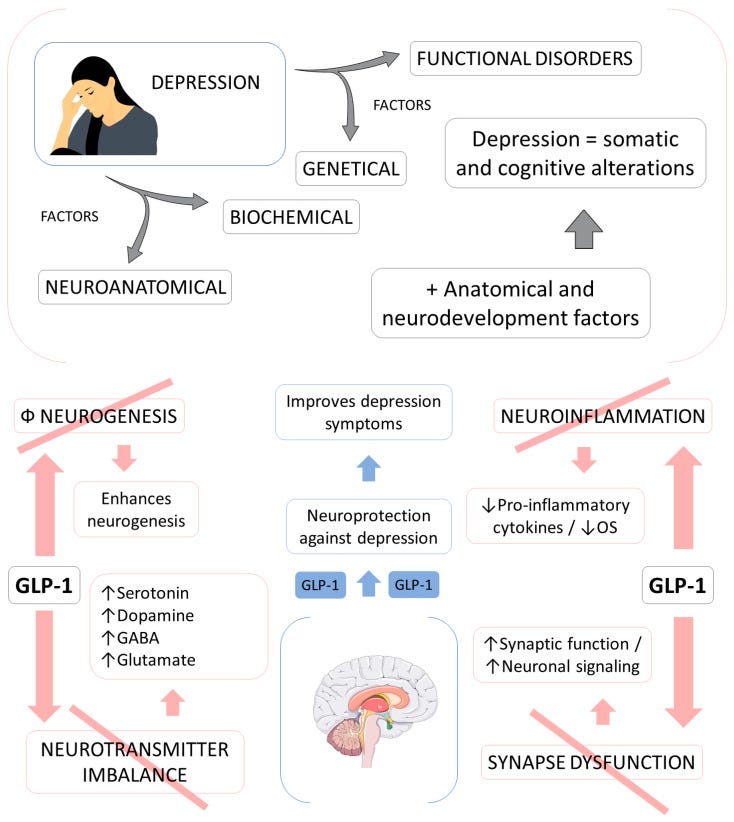
Overall, the proposed mechanisms of treating depression with GLP-1 RAs, aside from reductions in diabetes and obesity, seem to be rather multifaceted. So far clinical trials have been limited, with most trials of GLP-1 RAs as antidepressants being conducted in people with Type-II diabetes and therefore may be confounded by the direct actions of GLP-1 RAs on diabetes management. Nonetheless, there’s growing interest in figuring out many different uses of GLP-1 RAs. Some recent systematic reviews/meta-analyses have raised further considerations into this avenue of research as well.3
Unfortunately, with all this being said, we are still left with a curious question of why exactly suicidal ideation may be related with the use of these GLP-1 RAs.
Hopefully we get more answers in the future, but for now I’m curious if these drugs may be inducing effects similar to antidepressants such as selective serotonin reuptake inhibitors (SSRI), which are known to increase the risk of suicidal ideation in susceptible individuals (albeit this hypothesis is also seen as controversial).
To that extent, it’s possible that these reports of suicidal ideation may be the same as all of these other adverse events being reported. That is, there may be such a thing as too much of a good thing when it comes to these GLP-1 RAs, such that a subset of the population may hyper respond to these drugs which may lead to these reported adverse events.
It’s curious if some people may experience suicidal ideations at higher doses of GLP-1 RAs, or even if these drugs induce too strong of a release of neurotransmitters or synaptic function, thus leading to suicidal ideation.
More research needs to be conducted in order to figure out if these reports are clear signals or noise related to other circumstances, and more research will be needed to find mechanistic explanations for these adverse events.
But more importantly, more awareness needs to be made that these drugs are not merely antidiabetic or weight-loss drugs, but that these drugs are acting as hormones (and strong ones at that). There is plenty we have yet to uncover about native GLP-1, so who’s to say that more adverse events may not be reported as these drugs become more and more popular.
More awareness, more research, and more hesitancy should be practiced when looking at these, and other medications.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists such as myself to provide work outside of the mainstream narrative.

Detka, J., & Głombik, K. (2021). Insights into a possible role of glucagon-like peptide-1 receptor agonists in the treatment of depression. Pharmacological reports : PR, 73(4), 1020–1032. https://doi.org/10.1007/s43440-021-00274-8
Laurindo, L. F., Barbalho, S. M., Guiguer, E. L., da Silva Soares de Souza, M., de Souza, G. A., Fidalgo, T. M., Araújo, A. C., de Souza Gonzaga, H. F., de Bortoli Teixeira, D., de Oliveira Silva Ullmann, T., Sloan, K. P., & Sloan, L. A. (2022). GLP-1a: Going beyond Traditional Use. International journal of molecular sciences, 23(2), 739. https://doi.org/10.3390/ijms23020739
Chen, X., Zhao, P., Wang, W., Guo, L., & Pan, Q. (2023). The Antidepressant Effects of GLP-1 Receptor Agonists: A Systematic Review and Meta-Analysis. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry, S1064-7481(23)00394-9. Advance online publication. https://doi.org/10.1016/j.jagp.2023.08.010








Eeek. These, and SSRIs possibly linked to aggressive behavior... pharmaceuticals can be very dangerous and not to be taken lightly.
No link, of course, between the increasing availability of these "suicide" drugs and the fact that Canada and a number of other countries are pushing legal state euthanasia for all.