Taking Antihistamines for allergies?
A general look into antihistamines, and why you probably shouldn't wait for symptoms before you take them.
As we head into the twilight of summer and the emergence of fall some readers may experience begin to experience allergies (if they have not done so in the prior seasons).
Allergies during this time of year are apparently caused by species relating to Ambrosia, as Weedom posted out in one of their posts.
Please check out the article if you’re interested in ragweed (because why wouldn’t you be?).
Whether we call it hay fever, allergic rhinitis, or just seasonal allergies this somewhat benign immune response to foreign antigens has become rather common in the modern age.
It’s not too difficult to find articles detailing the increase in allergies worldwide. The real question becomes why allergy diagnoses are growing in numbers. Among more common hypotheses are that more sterility has led to an improperly trained immune system- a hypothesis called the hygiene hypothesis. It at least argues that children who live in more rural settings who also deal with a lot of outdoor work are exposed to more allergens early on in life, providing the body an ability to tolerate said allergens.

Another hypothesis points towards changing dietary habits that include more processed foods, which may explain the increase in food allergies. This may pair with exposure to environmental toxins as well as modern proclivities that may damage our microbiome and leave us more vulnerable.
This post, however, isn’t about the rise in allergies but rather the drugs we take to deal with seasonal allergies- antihistamines.
What do histamines do exactly, why are they produced by the body, and why don’t they work in the event of an allergic response?
We’ll take a rather broad dive into the world of antihistamines below. As always, remember that articles such as these are intended to be informative, not prescriptive.
What is Histamine?
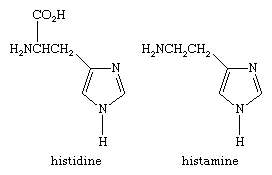
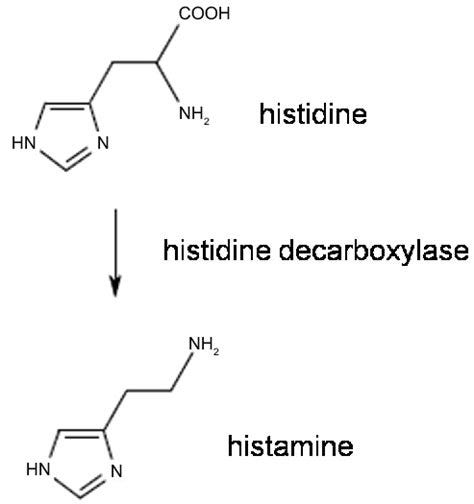
The history of histamine’s discovery is a rather interesting one. The name histamine sounds rather similar to a common amino acid called histidine. In fact, they share the exact same structure aside from the lack of a carboxyl group in histamine, thus the emphasis on it being an -amine.
One of the first studies to isolate histamine occurred with isolating the compound from ergot. When injected into animals various biological effects were noticed (Parsons, M. E., & Ganellin, C. R.1):
It is now almost one hundred years since Sir Henry Dale (Figure 1) and his colleagues at the Wellcome Laboratories isolated histamine from the mould ergot. They then went on to carry out a ground-breaking series of experiments to explore its biological actions. They found that it had a stimulant effect on smooth muscle from the gut and respiratory tract, caused vasodepression, stimulated cardiac contractility and induced a shock-like syndrome when injected into animals (Dale & Laidlaw, 1910; 1919). Popielski (1920) demonstrated that histamine had a marked stimulant effect on the secretion of acid from the stomach of dogs. In 1924, Lewis described the classic ‘triple response' to histamine consisting of a red spot due to vasodilatation, a wheal which was the consequence of increased permeability and flare due to an axon reflex (Lewis & Grant, 1924).
It wasn’t until a few years later that histamine would be isolated from liver and lung samples, suggesting that histamine is a compound normally found within the body, although the structural similarities to histidine raised questions as to whether this compound was just a metabolite of histidine and played no active role in the body.
Eventually, studies looking at individuals pre and post-anaphylaxis, as well as pre/post-septic shock would note elevated histamine levels relative to levels before the incident, adding further evidence of histamine playing a causative role in allergies and other physiological responses in the body.
How is Histamine produced?
Indeed, histamine is produced by the removal of a carboxyl group from histidine by way of none other than histidine decarboxylase2:
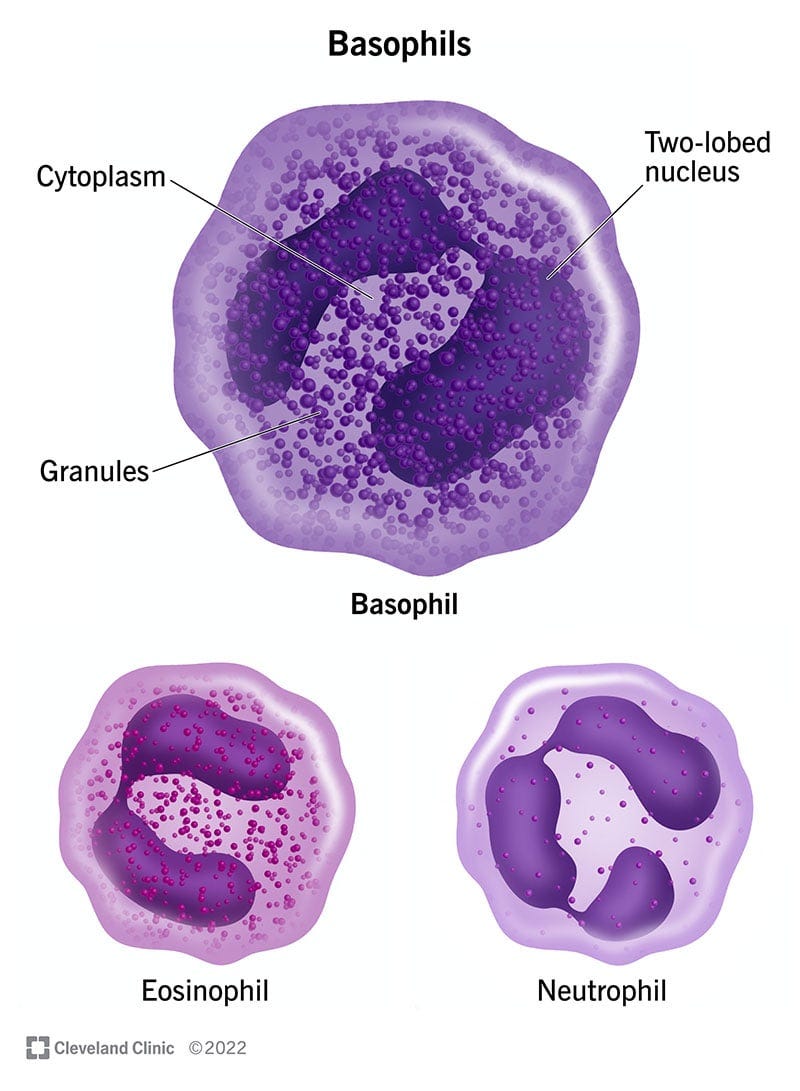
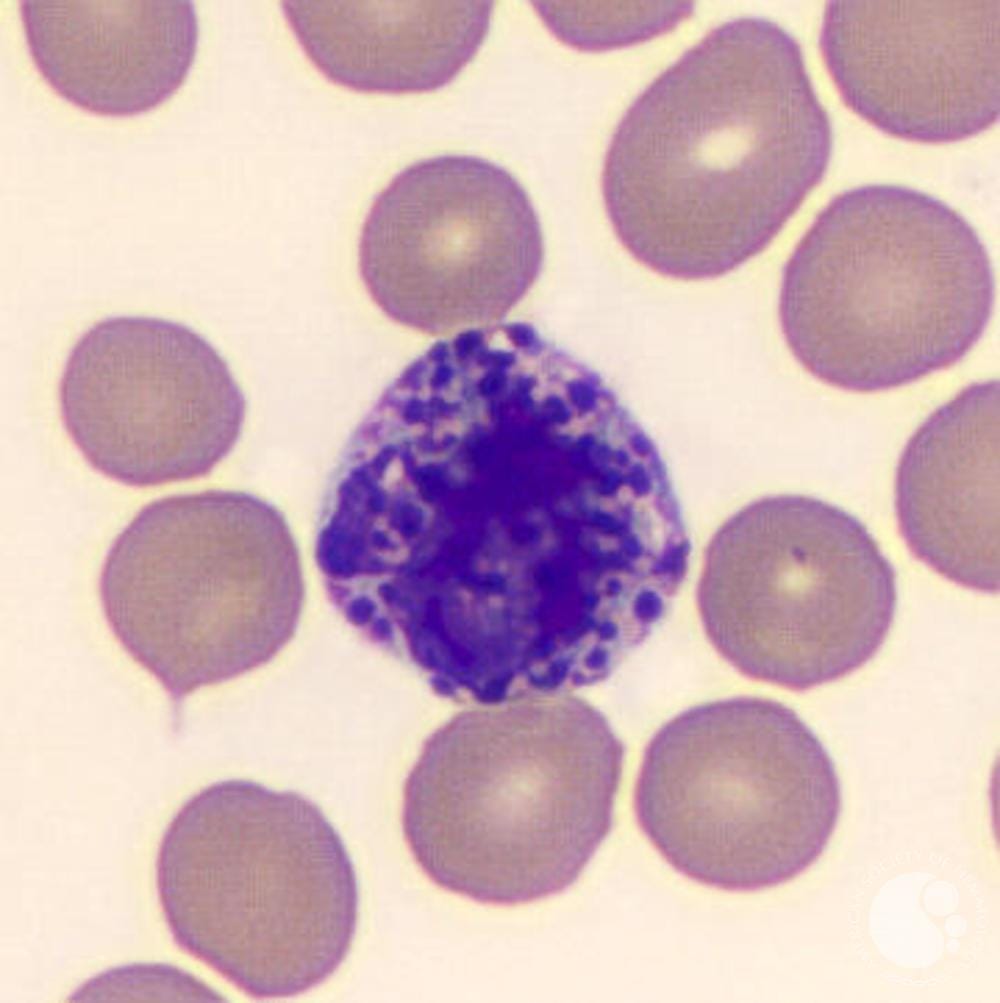
Several cell types express genes related to histidine decarboxylase formation, with the most commonly known cells being some granulocytes such as basophils and mast cells, which produce histamine intracellularly and store them within granules. This produces the spotty appearance of these cells when examined under a microscope.
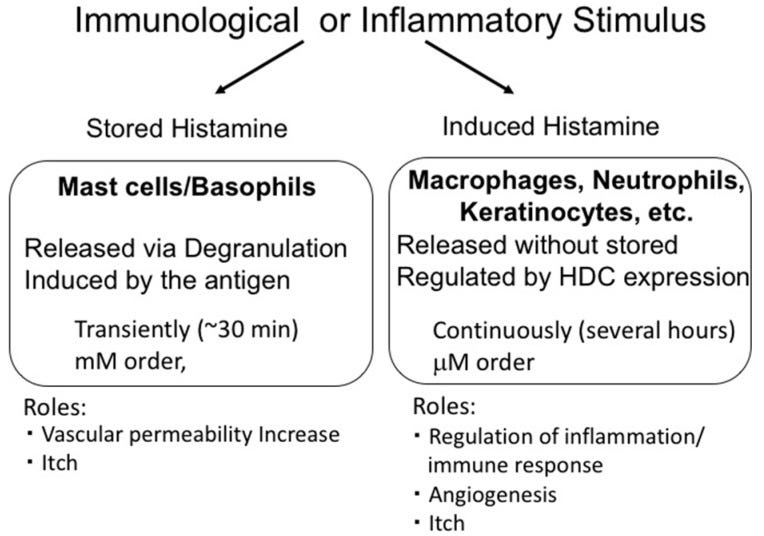
Other immune cells may be induced to produce histamine by way of inflammatory cascades rather than through the storage and release (degranulation) of histamine.
An overview of this process is provided by Hirasawa, N.3:
Histamine is synthesized from histidine by histidine decarboxylase (HDC) [24]. In mast cells and basophils, histamine is produced and stored in granules. The stored histamine is released via degranulation induced by immunological stimulation, such as that by antigens. This type of histamine release is induced rapidly and the histamine levels in surrounding tissues reach a concentration in the order of mM. In contrast, histamine production at inflammatory sites is induced slowly and continuously. In this case, histamine is synthesized de novo in various cells via HDC induction and is released without being stored. Such histamine is called ‘nascent histamine’ or ‘induced histamine’. Importantly, in this case, the levels of histamine in the tissues are limited to the µM range, suggesting that induced and stored histamine play different roles (Figure 1).
Surprisingly, histamine has also been found within the brain where it serves a different role, usually related to wakefulness and even goal-oriented behaviors, as well as other yet-to-be-discovered roles.4 We’ll explore this role of histamine within the brain a bit more further on.
Histamine Receptors
Overall, there appears to be 4 receptors that bind histamine, each with different roles within the body.
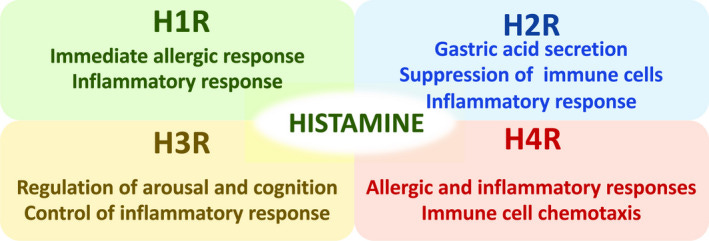
Within the context of allergies H1 receptors are usually what is being discussed. It’s one of the more ubiquitous histamine receptors (Moriguchi, T., & Takai, J.5):
Histamine H1 receptor (H1R) is globally expressed in various tissues, including bronchial smooth muscle cells and vascular smooth muscle cells. When histamine binds to H1R, it elicits airway contraction, vascular relaxation, vascular permeabilization and mucosal secretion. Consequently, the type I immediate allergic responses emerge, including bronchial asthma and anaphylaxis.
In contrast, H2R is predominately expressed within the stomach, H3R within the CNS, and H4R on the surface of various immune cells.
What happens during an allergic reaction?
The following overview is a gross simplification of the information provided by Wheatley, L. M., & Togias, A.6. Please refer to the article’s caption for a deeper view of the following figure and the events described below.
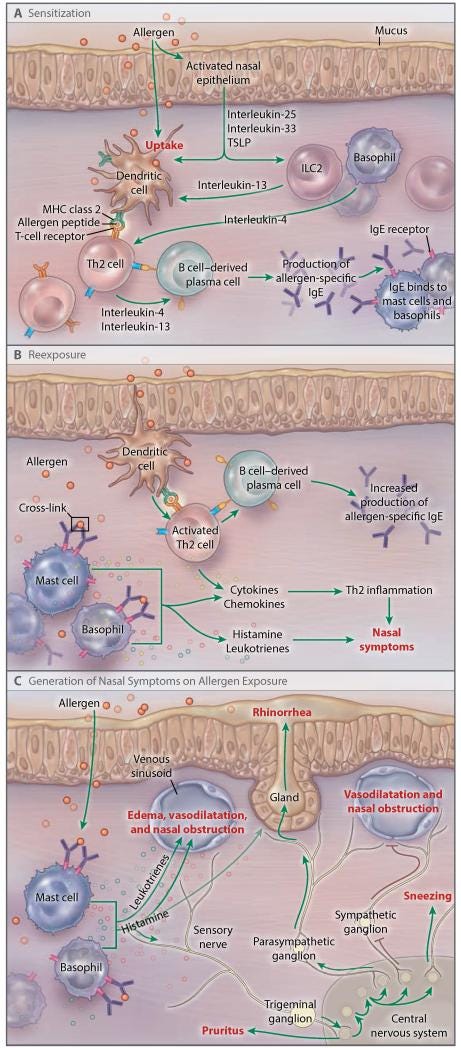
The events of an allergic response are rather straightforward, and are synonymous with initial exposure/sensitization followed by subsequent recognition of allergens. This process is similar to that of autoimmunity or even of infections, and so it’s interesting to consider this overlap in immunological processes.
In short, the initial sensitization process involves antigen-presenting cells such as dendritic cells, which bind these allergens and present them to T-cells. Recognition of these allergens result in further responses which result in the formation and release of IgE antibodies to target these allergens (Panel A).
For allergens in which the immune system has become sensitized, repeat exposure, usually by way of the nasal passages, will lead to binding of these allergens with IgE antibodies (Panel B).
These IgE antibodies can then bind to mast cells and basophils through effector function, directed by the Fc stalk of IgE antibodies binding to Fc receptors on these granulocytes. The result is the release of histamine, among other molecules which result in inflammatory responses and permeability of blood vessels (Panel C).
Normally, endothelial cells are kept tight by way of tight junctions formed between cells. But as inflammation increases the space between cells become more permeable, leading to the passage of fluid from blood vessels and lymphatic vessels into nearby regions. This comes as vasculature within the nearby area become enlarged as well, leading to obstruction of the nasal passage and anaphylaxis in some instances.
This is where the swelling from allergies comes from. As histamine continues to bind to H1 receptors the nasal symptoms of allergies develops within hours of exposure, leading to inflammation and swelling within the nasal passages- a phenomenon labeled as allergic rhinitis, with rhinitis referring to inflammation of the mucosal membranes within the nose.
It’s worth noting that at the time of inflammation exposure to other irritants or strong odors may also exacerbate symptoms related to allergic rhinitis.
It’s also important to note that, especially within the case of food allergies and animal venoms such as bee venom, that introduction of an allergen and the sensitization event may not lead to as severe of an event as re-exposure events. Be careful in assuming that an allergic response to a food allergen may be minor if it occurs during the sensitizing event, as subsequent responses are likely to be far worse and possibly even deadly if anaphylaxis occurs as the immune system is made more aware and more active in targeting the allergen at the time of re-exposure.
Preventing allergies- Antihistamines*
*Note that any reference to histamine receptors below refers specifically to H1 histamine receptors, as these are the main targets of antihistamines.
In conjunction with the development of medicinal chemistry, the discovery of histamines, and research into histamine’s role in allergies researchers began searching for ways to block histamine binding and prevent allergies.
There’s much to the history of antihistamine development, but in short antihistamines work in a rather interesting manner.
First off, it’s a bit improper to argue that antihistamines are histamine antagonists. Although some compounds may compete for histamine for binding on histamine receptors, it appears that the actual mechanism of action for antihistamines lie in turning “off” histamine receptors.
In short, histamine receptors are G-coupled protein receptors that exist in equilibrium between an “on” and “off” position. When histamine enters into the central core of H1 receptors it induces the receptor into the “on” position by interaction with certain domains and inducing a conformational change. Elevated expression of histamine would therefore lead to a bias for H1 receptors to exist in the “on” position, and therefore leading to the series of events associated with an allergic response.
In contrast, antihistamines lead to a bias towards these receptors in staying in the “off” position by binding to different domains within the receptor. These drugs are therefore not considered antagonists, but inverse agonists since they induce the opposite effect of histamine.
The development of antihistamines can be separated based on their generation and relationship to side effects.
First generation antihistamines were developed around the 1940s as a tangent to cholinergic antagonists, and likely is the reason for their pharmacological effects of sedation (Church, D. S., & Church, M. K.7):
Candidate antihistaminic compounds were primarily modifications of those synthesized as cholinergic antagonists and are from diverse chemical entities, ethanolamines, ethylene diamines, alkylamines, piperazines, piperidines, and phenothiazines. It is hardly surprising, therefore, that these first-generation antihistamines had poor receptor selectivity and significant unwanted side effects.
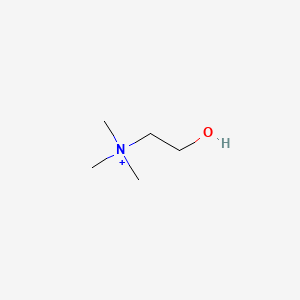
Compare the structure of choline and Diphenhydramine (commonly known as Benadryl), and you can see the structural similarities:

Here’s a list of first generation antihistamines for those interested8:
Many of these first generation antihistamines were poor antihistamine agents, and due to their structural similarity to choline could actively permeate the blood-brain barrier and enter into the central nervous system. This appears to be the reason for the sedative effects of these compounds. In contrast to the nasal mucosa, remember that histamine produced within the CNS is involved with wakefulness. Thus, any first generation antihistamines that enter into the CNS may inhibit histamine function and cause drowsiness (Church, D. S., & Church, M. K.):
Because first-generation H1-antihistamines derive from the same chemical stem from which cholinergic muscarinic antagonists, tranquilizers, antipsychotics, and antihypertensive agents were also developed, they have poor receptor selectivity and often interact with receptors of other biologically active amines causing antimuscarinic, anti-α-adrenergic, and antiserotonin effects. But perhaps their greatest drawback is their ability to cross the blood-brain barrier and interfere with histaminergic transmission. Histamine is an important neuromediator in the human brain which contains approximately 64,000 histamine-producing neurones, located in the tuberomamillary nucleus. When activated, these neurones stimulate H1-receptors in all of the major parts of the cerebrum, cerebellum, posterior pituitary, and spinal cord[15] where they increase arousal in the circadian sleep/wake cycle, reinforce learning and memory, and have roles in fluid balance, suppression of feeding, control of body temperature, control of the cardiovascular system, and mediation of stress-triggered release of adrenocorticotrophic hormone and β-endorphin from the pituitary gland[16]. It is not surprising then that antihistamines crossing the blood-brain barrier interfere with all of these processes.
It appears that histamine is released during the day and is involved with wakefulness. At night, histamine production declines and induces drowsiness.
This has led to some controversy given the CNS role of these first generation antihistamines, with some questions being raised about the use of these medications in children, possible consequences with long-term use, as well as their role in sedation if other compounds are not considered viable. Contraindicators for first-generation antihistamines should also be considered, as these compounds may interact synergistically with other drugs.
However, with growing interest in neurodegeneration some of these first generation antihistamines have found repurposed use in research, especially within the context of Parkinson’s disease, either alone or in conjunction with other treatments.9,10,11 This seems to be a recently emerging side of first generation antihistamines, so it would be interesting to see what further research makes of this repurposing.
It would take several decades until better antihistamines with no or reduced CNS involvement were developed. This second generation came about in the 1980s, and use of these antihistamines showed greater binding to histamine receptors while also showing poor blood-brain barrier permeability12.
In contrast to the structures of first generation antihistamines, second generation antihistamines are somewhat more bulky and with some bearing more complex ring structures:
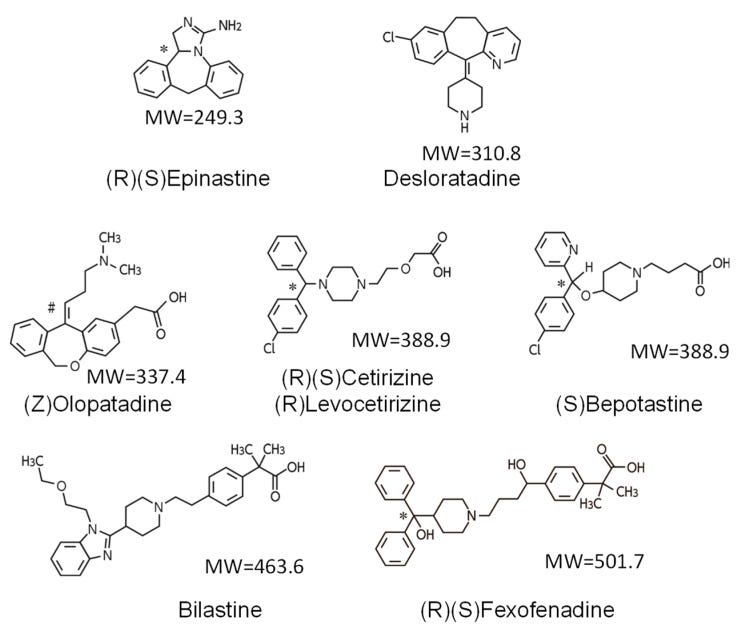
It should be noted that not all second generation antihistamines are non-sedative. Some even show interactions with muscarinic acetylcholine receptors. This effect is usually related to second generation antihistamines that bear amine groups such as Loratadine and Desloratadine. This effect doesn’t seem to appear with carboxyl-bearing antihistamines.
Given the concerns over the sedative effects, as well as other possible side effects of first generation antihistamines, these second generation compounds are generally considered safer and more effective. Their lack of sedative effects also make them far more appealing compounds as they can be used midday and early on without worry of drowsiness.
Some examples of second generation antihistamines can be found below:
Don’t wait to take an Antihistamine!
If you’re like me you likely wait until symptoms of allergies arise. It’s usually then you take an antihistamine, find out your allergies worsen and persist, and then lament the fact that these drugs do nothing to help reduce your allergy symptoms.
In reality, antihistamines are best suited as prophylactic medications. That is, they work best when used before an allergic reaction occurs.
If we follow the path from allergen exposure to allergic response, remember that at the time symptoms develop you have likely been exposed to the allergen in question for quite some time. IgE antibodies directed at these allergens have already been deployed, your basophils and mast cells have already been degranulated and have released histamine, and the flood of histamine is already likely binding to H1 receptors and locking them into the “on” position. After all, this is one of the reasons you would be experiencing symptoms in the first place!
All of these molecular events are likely occurring even before your symptoms arise and you decide to pop that antihistamine. At that point, these antihistamines can’t do much because the inundation with histamine likely doesn’t leave many H1 receptors free to be turned “off”, and so the end result is having all of these antihistamine molecules but nowhere to bind.
And so, if you’re someone experiencing some ragweed-related allergies, or any seasonal allergies, keep in mind that it’s best to deploy the antihistamines prior to the allergic reaction.
Substack is my main source of income and all support helps to support me in my daily life. If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists such as myself to provide work outside of the mainstream narrative.

Parsons, M. E., & Ganellin, C. R. (2006). Histamine and its receptors. British journal of pharmacology, 147 Suppl 1(Suppl 1), S127–S135. https://doi.org/10.1038/sj.bjp.0706440
Sahu, Lopamudra & Panda, Sandeep & Paramithiotis, Spiros & Zdolec, Nevijo & Ray, Ramesh. (2015). Biogenic Amines in Fermented Foods: Overview. 10.1201/b19872-18.
Note that my inclusion of this citation is more for the image rather than the content of this article which I haven’t examined.
Hirasawa N. (2019). Expression of Histidine Decarboxylase and Its Roles in Inflammation. International journal of molecular sciences, 20(2), 376. https://doi.org/10.3390/ijms20020376
Passani MB, Panula P and Lin J-S (2014) Histamine in the brain. Front. Syst. Neurosci. 8:64. doi: 10.3389/fnsys.2014.00064
Moriguchi, T., & Takai, J. (2020). Histamine and histidine decarboxylase: Immunomodulatory functions and regulatory mechanisms. Genes to cells : devoted to molecular & cellular mechanisms, 25(7), 443–449. https://doi.org/10.1111/gtc.12774
Wheatley, L. M., & Togias, A. (2015). Clinical practice. Allergic rhinitis. The New England journal of medicine, 372(5), 456–463. https://doi.org/10.1056/NEJMcp1412282
Church, D. S., & Church, M. K. (2011). Pharmacology of antihistamines. The World Allergy Organization journal, 4(3 Suppl), S22–S27. https://doi.org/10.1097/WOX.0b013e3181f385d9
The list for first generation and second generation antihistamines can be found from this review article:
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Antihistamines. [Updated 2017 Jan 16]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547896/
Tandra, G., Yoone, A., Mathew, R., Wang, M., Hales, C. M., & Mitchell, C. S. (2023). Literature-Based Discovery Predicts Antihistamines Are a Promising Repurposed Adjuvant Therapy for Parkinson's Disease. International journal of molecular sciences, 24(15), 12339. https://doi.org/10.3390/ijms241512339
Zhu, J., Ma, R., & Li, G. (2023). Drug repurposing: Clemastine fumarate and neurodegeneration. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie, 157, 113904. https://doi.org/10.1016/j.biopha.2022.113904
Ayaz, M., Anwar, F., Saleem, U., Shahzadi, I., Ahmad, B., Mir, A., & Ismail, T. (2022). Parkinsonism Attenuation by Antihistamines via Downregulating the Oxidative Stress, Histamine, and Inflammation. ACS omega, 7(17), 14772–14783. https://doi.org/10.1021/acsomega.2c00145
Kawauchi, H., Yanai, K., Wang, D. Y., Itahashi, K., & Okubo, K. (2019). Antihistamines for Allergic Rhinitis Treatment from the Viewpoint of Nonsedative Properties. International journal of molecular sciences, 20(1), 213. https://doi.org/10.3390/ijms20010213



Ya, pre-tuning before the flood of histamine is helpful. Herbalists caught onto this idea, and advise people to pre-tune prior to their allergy season with the herbs that show antihistamine effects. Some also emphasize the care and maintenance of a 'happy' liver, which is a major locus of histamine clearance through methylation.
This is fascinating info. I've had terrible 'all year allergies' to grasses, weeds and dust my whole life...I feel like a 'snot machine' (lol).
One thing that has helped mitigate some of my allergies is switching to homemade cotton handkerchiefs. I basically cut up a few worn out cotton dresses and I wash them with white thyme oil to clear any germs out.