Recent CDC data shows large majority of monkeypox hospitalizations in those with HIV/AIDS
Evidence indicates large portion of monkeypox cases within those with HIV or with prior evidence of STIs.
Edit: Grammar has been cleaned up and corrected in the article.
Last week the CDC published a report suggesting that nearly 82% of the monkeypox hospitalizations recorded were in those who were HIV+.
The CDC report summarized the findings of over 57 individuals who were hospitalized with severe monkeypox infection based on a collection of hospital records between the months of August 10- October 10, 2022.
The information can be summarized below:
Of the 57 individuals included in the summary 47 (82%) of the individuals were HIV+. Shockingly, only 4 of the 47 individuals (9%) were taking antiretrovirals at the time (emphasis mine):
This report summarizes findings from CDC clinical consultations provided for 57 patients aged ≥18 years who were hospitalized with severe manifestations of monkeypox¶ during August 10–October 10, 2022, and highlights three clinically representative cases. Overall, 47 (82%) patients had HIV infection, four (9%) of whom were receiving antiretroviral therapy (ART) before monkeypox diagnosis. Most patients were male (95%) and 68% were non-Hispanic Black (Black). Overall, 17 (30%) patients received intensive care unit (ICU)–level care, and 12 (21%) have died. As of this report, monkeypox was a cause of death or contributing factor in five of these deaths; six deaths remain under investigation to determine whether monkeypox was a causal or contributing factor; and in one death, monkeypox was not a cause or contributing factor.**
HIV is a virus that eats away at one’s immune system, with many deaths coming from coinfections from other pathogens due to the lack of being able to mount a proper immune response.
The information here is rather telling, as it indicates that a large portion of these individuals who have gotten severely ill likely couldn’t mount an immune response due to their HIV infection and the possibility of having AIDS.
If we look at Table 2, we’ll note that this too appears to be the case. AIDS is generally diagnosed when one has a CD4 count below 200 cells/uL.
The table suggests that 40 of the 47 HIV+ individuals would have CD4 levels low enough to be considered to have a diagnosis of AIDS. Note that 4 of these individuals were on antiretrovirals, and appeared to have their HIV infection under control (that leaves only 3 people with decent CD4 counts):
Also, if you were curious about some of the other individuals who were not HIV+, some of them were categorized as having a condition that would make them immunocompromised: three received solid organ transplants in the past and two were on chemotherapy. One of those receiving chemotherapy was also HIV+, so that would explain the 51 instead of the 52 as the person may not have been counted twice.
This information provides some explanation as to how the cases of monkeypox appear to culminate around gay men, as it’s likely that the circumstances of some of these men (i.e. being HIV+) may have made them far more susceptible.
This doesn’t take into account the fact that the outbreaks came about at a time where plenty of pride parades and events were occurring, although this likely created a viable place for the virus to spread rampantly among many gay men, especially if many of them had uncontrolled HIV and engaging in promiscuous activities.
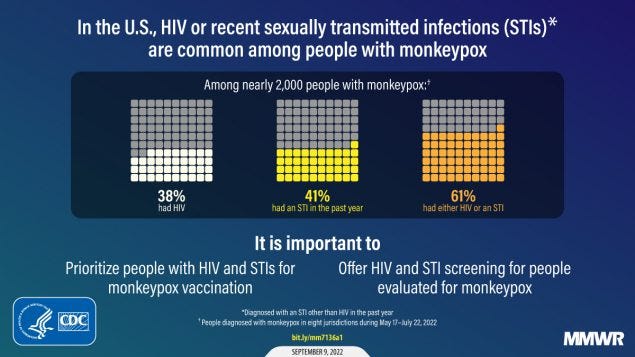
This builds off of a report from September which suggested that over 61% of those infected with monkeypox were also either HIV+ or were infected with STIs:
The September report includes the following:
Among 1,969 persons with monkeypox during May 17–July 22, 2022, HIV prevalence was 38%, and 41% had received a diagnosis of one or more other reportable STIs in the preceding year. Among persons with monkeypox and diagnosed HIV infection, 94% had received HIV care in the preceding year, and 82% had an HIV viral load of <200 copies/mL, indicating HIV viral suppression. Compared with persons without HIV infection, a higher proportion of persons with HIV infection were hospitalized (8% versus 3%). Persons with HIV infection or STIs are disproportionately represented among persons with monkeypox.
What’s interesting is that the rate of HIV/monkeypox coinfection increased as time went on since the initial outbreak, and older individuals showed a higher prevalence of HIV coinfection:
Among persons with monkeypox, the weekly percentage with concurrent HIV infection increased over time (31%–44% by July). The percentage of persons with monkeypox who had HIV infection was higher in older age groups: among persons aged 18–24 years, HIV prevalence was 21%, and among those aged ≥55 years, was 59%. HIV prevalence among persons with monkeypox also varied by race and ethnicity, ranging from a high of 63% among non-Hispanic Black or African American (Black) persons, to 41% among Hispanic or Latino (Hispanic) persons, 28% among non-Hispanic White persons, and 22% among non-Hispanic Asian persons.
Altogether, the information here presents a rather dark story. The fact that monkeypox was occurring concurrently with HIV and other STI’s points to concerns about the spread of other diseases as well.
It’s likely that those who may have gotten monkeypox, which would be rather mild for those competent immune systems, may be exposed to HIV as well.
I’ve been a bit critical in some of the coverage over monkeypox over the fact that many reports seemed to use the outbreak as a a way to criticize gay men for their lifestyle choices.
At the same time, the media didn’t do itself any favors by acting as if the spread of the disease coinciding during pride events didn’t have any association, or that pride itself has been heavily criticized for its portrayal of the LGBT community.
It’s far too hypocritical to argue that our lives needed to be halted at the onset of COVID but allow widespread festivities for a virus that has far more manageable control measures.
Stephanie Brail covered this topic a few months back where she discussed a man who, by all accounts, should have known better than to have slept with multiple men, only to result in him getting a triple infection of monkeypox, gonorrhea, and bacterial tonsillitis:
As I commented in that post—with similar sentiments from Stephanie— the main issue wasn’t that these were gay men, but the fact that all of this suggests continuous promiscuity among a select number of people likely owing to the start and spread of the outbreak, among possible outbreaks of HIV and other STI’s.
It almost rings similar to the sentiments about “hugging an Asian” at the start of COVID which, paradoxically was intent on providing a message of inclusivity and antiracism even it worked counter to the messaging on preventing COVID. Even as an Asian person myself I found all of the messaging to have been cringey and offensive in their own regard— you can keep your hugs to yourself Nancy Pelosi.
It’s even more concerning given the fact that HIV generally requires several years before it leads to AIDS. Many of these men likely were unaware of their HIV status, and a few who were may not have been on antiretroviral therapy.1
However, I found it fitting to cover this story as many reports at the time were also suggesting a possible association with the COVID vaccines and possible VAIDS (vaccine-induced AIDS).
Although such associations can’t be (and shouldn’t be) discounted, the fact that this became the prime consideration among skeptics was rather concerning, mostly because such narratives tend to muddy any possible alternatives.
Rather than look at all possible factors, reports would quickly be met with comments about this being related to the COVID vaccines.
Note that nearly a quarter of the severe cases of monkeypox occurred in the homeless (13, or 22%). The CDC report even mentions things along the lines of inequity in resources and care for the homeless.
If that can be said for homeless people with HIV/monkeypox, it’s probably not likely that these individuals would also be in consideration for COVID vaccines as well (however, personal accounts for each individual’s homeless status as it relates to medical history, including vaccination history, should not be discounted).
And so the evidence here provides a causative explanation. It may help to provide evidence as to why many gay men were being infected with monkeypox and may explain the deaths and severe outcomes in a select few individuals.
So far the evidence suggests an association between HIV infection/AIDS and severe outcomes from monkeypox, owing to the immunocompromised state of those infected.
Note that the evidence doesn’t explain the number of outbreaks, although the high level of STI’s may suggest a clear behavioral relationship.
As to the strange level of mutations found in this strain of monkeypox, it could be that serial passage through immunocompromised individuals may have led to opportunities for mutations to arise, although this would be a spurious assumption without any additional information.
It’s important to remember to look at all possible factors. Even if the vaccines shouldn’t be discounted, we should be careful in immediately assuming that everything we see is a consequence of the vaccines, especially if it prevents us from looking at other explanations.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

The October report includes 3 cases of men who were not on therapy for HIV.
Patient A: A Hispanic or Latino man in his 20s who was diagnosed with HIV in 2020 with no follow-up, suggesting possible lack of treatment. He would later succumb to monkeypox with an autopsy showing perfuse spread of monkeypox.
Patient B: A black man in his 30s with AIDS and not receiving treatment was diagnosed with monkeypox. He was also tested and treated for gonorrhea, syphilis, and chlamydia. He was still hospitalized at the time of the report.
Patient C: A white man in his 40s who also had AIDS and was not receiving treatment. Monkeypox eventually led to necrosis and amputated of extremities such as a toe and the man was still receiving treatment (including antiretrovirals) at the time of the report.





Is anyone even mildly surprised by these findings? I'm certainly not. But thanks for reporting them.
Thank you for your deep and skeptical look and a very interesting report. A very engaging article.
As a Covid writer, I used to frequent the /r/monkeypoxpositive subreddit when monkeypox was still a thing. The boils and pustules that monkeypox produces are super nasty!!!
Monkeypox is not particularly infectious. So, to spread it, you need large anonymous oral/anal group sex session with no protection used. Or dirty unwashed people copulating in homeless tent cities and selling cheap tricks under the bridge.
HIV is similar. You don't get it from a handshake -- it spreads through rough anal sex, shared needles, nasty behaviour etc etc.
Is this a surprise that many of the resulting sufferers of monkeypox have HIV?
Nevertheless, great find and I believe you found a real cause and effect relationship.