On my last post a few comments pointed out that my definition of a leaky vaccine was confusing and that a lot of the information may have gone over people’s heads.
So this post will serve to clarify what a vaccine is. Hopefully this information will provide the proper context to examine what makes a vaccine “leaky”.
Defining “Vaccine”
Of course, I probably should not have gone into describing what a “leaky” vaccine is before describing what a vaccine is!
When someone becomes exposed to an infectious pathogen such as a virus, bacteria, or parasite, they may undergo all forms of disease states. Sometimes it can be very mild and the infected person can recover quickly. Other times it may become severe and result in hospitalization and even death.
In cases where the disease progression does not lead to death, our bodies have evolved over numerous successive generations in order to recognize pathogens and make sure that we do not become ill again.
That process relies on our immune system, which is a collection of various cells, organs, tissues, and biochemical pathways that are intended to protect us from exogenous (foreign) entities that may harm us. Some of those immune cells responsible are listed below, but note that this post will not dive into the inner machinations of immune function. But for those who would like an article on the immune system you can find one here1.

But let’s be real: most people would rather not get sick in order to gain eventual immunity from a pathogen, and you certainly don’t want to test fate when the infectious agent has a high probability of leading to death.
If there was a way for one to gain immunity without all the hassle and hazards of falling ill, then there’s a huge possibility of saving millions of people from having to needlessly suffer in order to confer immunity.
That’s where vaccines come into play.
Vaccines are prophylactic (preventative) treatments that are intended to elicit an immune response without all of the worries of falling deeply ill.
But in order to conduct such a feat, a person has to be exposed to the intended antigen in some way in order for the immune system to know what it must protect against.
Vaccine Platforms
First iterations of vaccines took the active pathogen and inoculated2 (exposed) recipients to the inoculum. In order to vaccinate against smallpox, a method was used called variolation in which tissue, skin, and puss from an infected smallpox skin legion was placed onto a needle and administered (inoculate) to a recipient.
The intent with such a method was to provide just enough of the pathogen in order for a person’s immune system to kick in and create an immune response against the smallpox virus.
In some cases recipients would produce a minor smallpox infection until the immune system kicks in and cleared out the virus without much disease progression. However, in other variolation recipients the disease progressed and became severe or even lead to death.
The caveat of using a live pathogen is that it still has the capabilities to replicate and spread. Therefore, the possibilities of an infection boils down to how quickly and robustly a person’s immune system can clear the pathogen. In immunocompromised individuals their immune response may be greatly truncated or slowed down, leaving them vulnerable to severe disease due to their immune system’s inability to clear the infectious agent out.
From Pollard, A. J. & Bijker, M. E.3 (I will reference this article a lot):
Live vaccines are developed so that, in an immunocompetent host, they replicate sufficiently to produce a strong immune response, but not so much as to cause significant disease manifestations (for example, the vaccines for measles, mumps, rubella and rotavirus, oral polio vaccine, the Mycobacterium bovis bacillus Calmette–Guérin (BCG) vaccine for TB and live attenuated influenza vaccine). There is a trade-off between enough replication of the vaccine pathogen to induce a strong immune response and sufficient attenuation of the pathogen to avoid symptomatic disease.
Future vaccine technology would eventually utilize an attenuated pathogen where the pathogen’s replicating capabilities have been slowed down in order to slow down disease progression. Unfortunately, these attenuated pathogens are still able to replicate and may still be detrimental to immunocompromised individuals, albeit not to the same extent as intact viruses.
After years of further research, vaccinology- the study of vaccines, has come up with many different forms of vaccines that do not utilize an infectious agent.
Some include an inactivated virus which has no replicating capabilities but still provides the whole virus to a recipient’s immune system which can then recognize it. There are also antigenic vaccines which take immunogenic4 fragments of a virus or bacteria and introduce it to a recipient in order to elicit an immune response to those antigens, with the hope that partial training of the immune system may still confer a broad level of protection against the pathogens from which the antigens were derived.
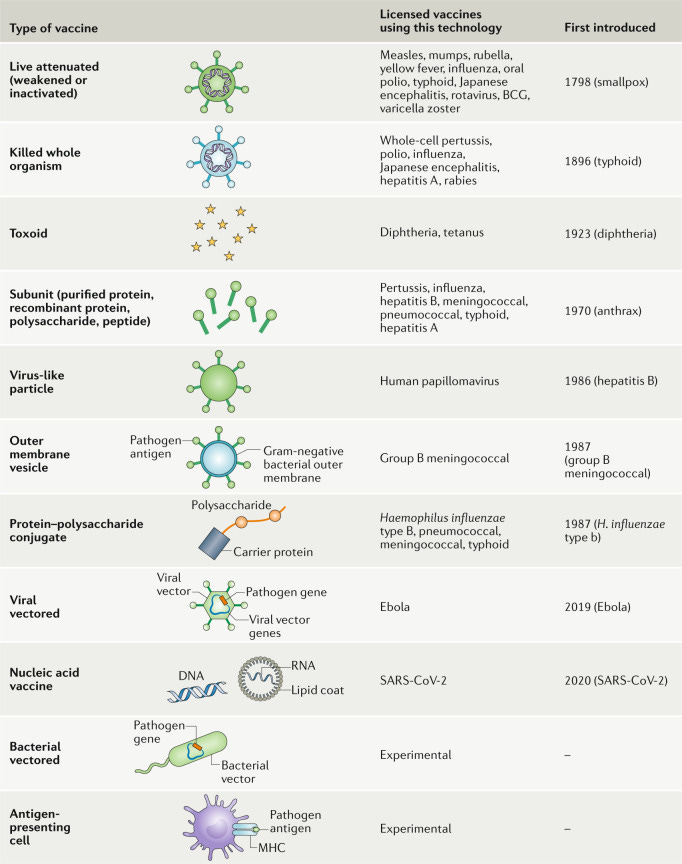
Several variations of vaccines can be seen below (Pollard, A. J. & Bijker, M. E.):
The overall intent of a vaccine can be boiled down into two concepts:
Produce antibodies that can target and neutralize the intended pathogen
Create an immune memory that protects against future infections
Antibody Production
One of the main intentions of vaccine is to produce antibodies. Antibodies are small protein molecules usually depicted in a Y-shape. The top of the Y-prongs are the important regions of antibodies. These regions are called variable regions because the amino acid sequence of this region varies between antibodies.

Because different antibodies have their own array of amino acid sequences, antibodies have a specificity towards the various parts of an antigen. Regions of an antigen where antibodies can stick are called epitopes, and it is the interaction between the variable antibody regions (also called paratopes) and epitopes that are important to an antibody’s function.
These interactions are usually based on electrostatic interactions such as ionic (positive/negative interactions), hydrogen bonding, and polar interactions.
For example, let’s say an epitopic region of an antigen is full of negatively-charged amino acids. A perfectly antibody for this region would be on that complements the high level of negative charge- such an antibody would have a positively-charged variable region.
The two opposites would attract, and the interaction would cause the antibody to bind to the epitope.
So in essence, antibodies have to complement the epitopes they bind to through a favorable attachment5.
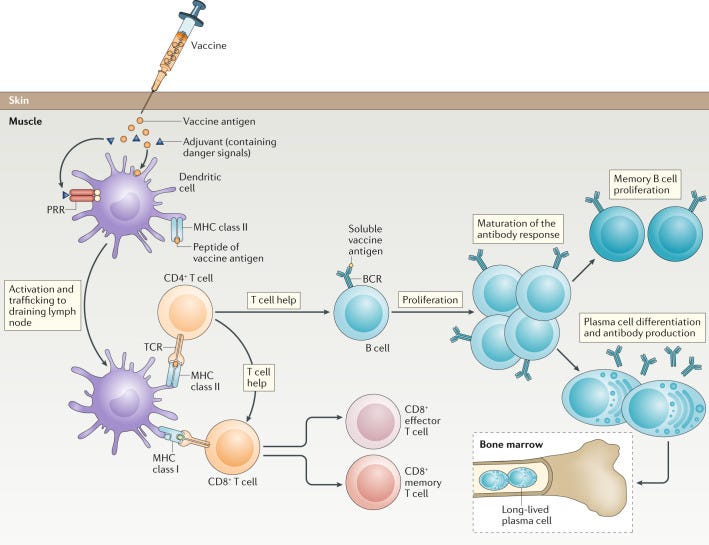
When someone is presented with antigens- whether from a vaccine or a pathogen- a cascade of events leads to the production of antibodies, all of which can complement and bind to the antigen and prevent it from causing harm. If antibodies bind to regions of a pathogen, such as a virus, that prevents the virus from entering and infecting cells, that antibody is considered a neutralizing antibody since it completely stops the virus.
The antibody production process is illustrated below. Note that the antibodies are what’s important, so I won’t go into detail into what goes on inside the immune cells.
What’s important to remember is that the lifespan of antibodies vary greatly. Whether they last weeks or months, remember to keep in mind one thing- producing antibodies takes time and energy. When the body is not constantly inundated by the same pathogen, it may reduce antibody production instead of wasting resources. In that regard, we can see why antibodies are not the end-all/be-all of immunity. Instead, we hope that our bodies are able to remember an infection and respond appropriately years down the line.
Immune Memory
There’s no use in having an immune response that only works at the point of infection- we probably wouldn’t have lasted as long as a species if we didn’t have a way of both dealing with a pathogen as well as remember it in case we come across it again.
It’s important that immunity also remembers and recognizes pathogens. Essentially, we should have long-term protection through immune memory.
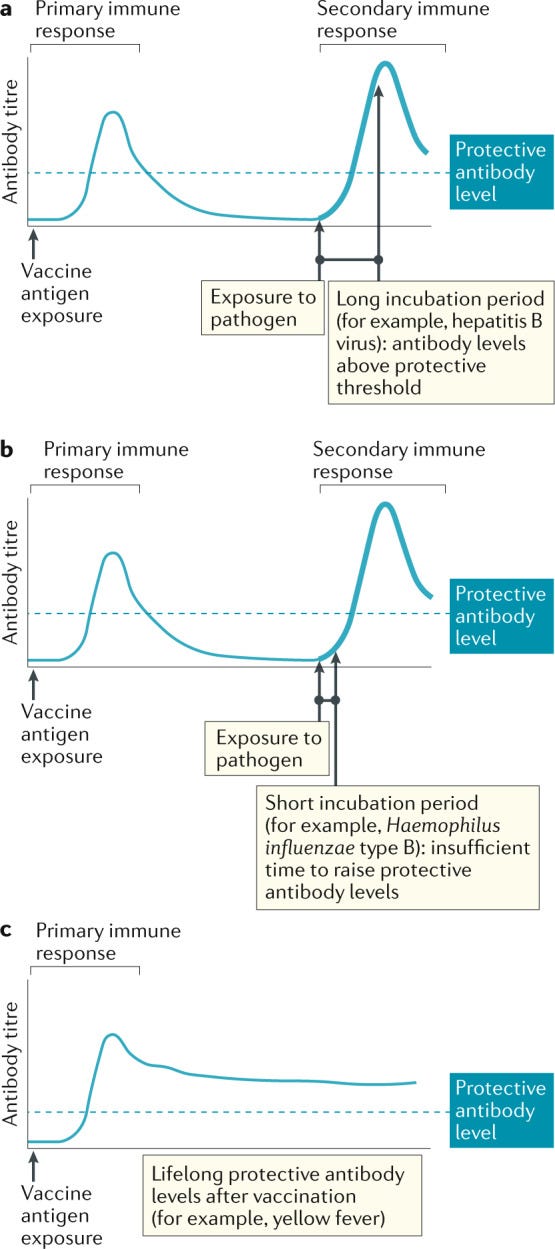
Immune memory refers to the immune system’s ability to respond quicker and more efficiently against a pathogen that it has already experienced. Unlike antibodies, which may circulate for weeks or months within the body and halt active infections, immune memory relies on the immune system’s ability to recall and react even years after to a previously introduced pathogen.
The effect here is presumed to be two-fold. One, the immune system should quickly and effectively deal with successive pathogen/antigen presentations. Secondly, the antibody production the second time around should be even greater and more robust. Ideally, vaccination should provide enough protection to reduce severity of illness, with a subsequent natural infection leading to an even more robust immune response.
In that regard, immune memory is contingent upon the incubation period of an infection, which is the time between an initial infection and the onset of symptoms.
Vaccine Efficacy
What does it mean when one considers a vaccine to be effective? Should it reduce transmission? Or should it reduce symptoms and severity of illness? Should a vaccine only protect the recipient or should it indirectly protect others? Or maybe a vaccine should do all of the above?
Vaccine effectiveness and efficacy can really refer to a host of different variables to consider. Even the terms “effectiveness” and “efficacy” may indicate different things.
Here’s an excerpt describing the differences, as well as additional terms( Shim, E. & Galvani, A. P.6, emphasis mine):
The interchangeable use of terms used to measure and parameterize vaccine efficacy and effectiveness can lead to inaccurate parameterization of epidemiological models and needs to be made explicit. Vaccine efficacy measures the protective effects of vaccination by the reduction in the infection risk of a vaccinated individual relative to that of a susceptible, unvaccinated individual [2]. In contrast, depending upon the study design of clinical trials, population-level vaccine effectiveness can be further categorized into the ‘direct’, ‘indirect’, ‘total’ and ‘overall’ impact of the vaccine [2–4] (Figure 1). Halloran et al. presented a seminal framework relating the different vaccination effects relevant study designs [5]. Direct effects compares the direct risk of a randomly selected individual with and without the vaccination program [1]. Indirect effects can be estimated from the difference in the degree of protection that unvaccinated individuals receive in the presence versus the absence of a vaccine program. ‘Total’ effectiveness measures the relative infection risk in vaccinated individuals compared to the infection risk in unvaccinated individuals before a vaccination program is launched [6]. Thus, ‘total’ effectiveness of vaccination is the effect of the vaccination program combined with the effect of the person having been vaccinated [5]. However, ‘total’ effectiveness does not take into account indirect protection of unvaccinated individuals in partially vaccinated population. ‘Overall’ effectiveness of a vaccination program is defined as the reduction in the transmission rate for an average individual in a population with a vaccination program at a given level of coverage compared to an average individual in a comparable population with no vaccination program [5, 6]. Thus, the ‘overall’ effectiveness takes into account benefits accrued by both vaccinated and unvaccinated individuals, and it is the measure most commonly used to evaluate the impact of a mass vaccination program at the population level [7, 8].
The terms “vaccination program” can get confusing, but several researchers suggest that efficacy refers to ideal settings while effectiveness refers to real-world settings when conducting clinical trials. Refer to Singal, et. al.7 for additional information.
When considering how “effective” a vaccine is, keep in mind that factors such as transmissibility, infectiousness, level of immunity, and the pathogen itself all affect how well a vaccine works. Essentially, a real-world setting will alter the course of a vaccine’s effectiveness. Take into account the figure from Friday’s post (link at the top) and how all of these factors alter a vaccine’s effectiveness. Always remember that most mentions of vaccines tend not to take into account these variables, and thus generally do not provide a good picture into what happens when one gets vaccinated.
Herd Immunity
Edit 6/22/2022: I missed the word just in the following sentence which changed that sentence’s meaning. Apologies for missing that!
Vaccines, and immunity as a whole, do not confer protection in just those that receive them. If immunity has the ability to reduce transmission and infectiousness, then a high level of immunity within a population may lead to the eventual eradication of a pathogen.
This form of immunity is referred to as herd immunity, in which many people within a given population become protected from a pathogen, and thus preventing its ability to spread while also protecting those who may be either immunocompromised or naïve to the pathogen (Pollard, A. J. & Bijker, M. E., emphasis mine):
Although direct protection of individuals through vaccination has been the focus of most vaccine development and is crucial to demonstrate for the licensure of new vaccines, it has become apparent that a key additional component of vaccine-induced protection is herd immunity, or more correctly ‘herd protection’ (Fig. 5). Vaccines cannot protect every individual in a population directly, as some individuals are not vaccinated for various reasons and others do not mount an immune response despite vaccination. Fortunately, however, if enough individuals in a population are vaccinated, and if vaccination prevents not only the development of disease but also infection itself (discussed in more detail below), transmission of the pathogen can be interrupted and the incidence of disease can fall further than would be expected, as a result of the indirect protection of individuals who would otherwise be susceptible.
Remember that immunity is derived from natural immunity as well, and thus herd immunity should take into account both forms of immunity.
When enough people acquire immunity a population would be considered to have reached herd immunity status. In order to reach “herd immunity status”, the level of immunity among a given population must be high enough to prevent a pathogen from circulating among the population, which usually depends on the contagious nature of the pathogen. This means that “herd immunity status” is entirely contingent upon how a virus operates and how good the immunity is at protecting against said pathogen.

Vaccines may seem simplistic in nature, but the entire process is rather complex and has not been fully elucidated. Many people may now have consternation in regards to COVID vaccines, but note that this review is intended to provide a general overview. However, this information can be used to relate to the COVID vaccines, as well as illustrate where COVID vaccines may have gone wrong.
That will be explained further in another post on Vaccine Failures and will provide more context to the phrase “leaky vaccine”.
Nicholson L. B. (2016). The immune system. Essays in biochemistry, 60(3), 275–301. https://doi.org/10.1042/EBC20160017
Along with the term inoculated comes the term inoculum, which refers to the substance that one is intended to be inoculated with. Vaccines are considered to be a form of an inoculum, and so too is exposure to a pathogen.
Pollard, A. J., & Bijker, E. M. (2021). A guide to vaccinology: from basic principles to new developments. Nature reviews. Immunology, 21(2), 83–100. https://doi.org/10.1038/s41577-020-00479-7
This is a good, general overview of vaccinology.
Both the words antigen and immunogen are portmanteaus with the suffix of both being derived from the word generator. Thus, antigen is a portmanteau of antibody generator, and refers to something that produces antibodies. Following along those same lines, immunogen is something that produces an immune response (immune generator).
Note that this relationship also extends to antigen/receptor binding, such that opposite, favorable interactions lead to proper binding between the two. Such a relationship may cause one to assume the transitive property may be at play: if there is an antigen/receptor relationship, and there is also an antibody/antigen relationship, then we may assume there is an antibody/receptor relationship. In part, this may be true. For example, the example of the highly negative epitope of an antigen may mean that both the receptor and antibody amino acid sequence may be positively charged. This idea doesn’t always hold up, but it at least indicates that there may be slight relationships between receptors and antibodies.
Shim, E., & Galvani, A. P. (2012). Distinguishing vaccine efficacy and effectiveness. Vaccine, 30(47), 6700–6705. https://doi.org/10.1016/j.vaccine.2012.08.045
Singal, A. G., Higgins, P. D., & Waljee, A. K. (2014). A primer on effectiveness and efficacy trials. Clinical and translational gastroenterology, 5(1), e45. https://doi.org/10.1038/ctg.2013.13





I missed this post originally, but thankfully I read it and it is incredible. A high-effort, informative, and very good introduction overall. Thanks for taking your time to write it ,.
Perhaps your previous post was somewhat leaky... :)