Hydroxychloroquine: An Overview
Part I: History and General Medicinal Properties
Hydroxychloroquine has been part of the mainstream discourse since the beginning of the pandemic, with many countries adopting it’s usage at the beginning of the pandemic.
However, the evidence around Hydroxychloroquine’s efficaciousness was murky, and unfortunately the utterance of the word by then President Donald Trump caused many to speak out against the drug.
More importantly, there were large reports of possible cardiotoxicity with the use of the drug, concerns that seemed to later be validated with a report in the Lancet, a premiere medical journal, indicating the ineffectiveness of HCQ against COVID as well as the cardiotoxic side effects.
As many are aware by now, the Lancet piece has been debunked (it’s probably a good idea to not lie about COVID hospitalizations in areas where an outbreak did not occur yet), and yet the narrative around the dangers of HCQ have persisted.
We have seen many claims about the toxicity/ineffectiveness of several different drugs throughout the pandemic, and if we are to arm ourselves against any forms of misinformation we need to have a general idea about these topics.
So here I’ll provide a general overview of Hydroxychloroquine by going over a brief history, its clinical uses, and its possible mechanism of action against SARS-COV2. Then, in my paid only Substack piece, I’ll discuss how many of the claims against HCQ and COVID may be overblown, or are in need of context.
Note that I may interchange studies that cite Chloroquine instead of Hydroxychloroquine, but know that HCQ operates the same way and studies that look at Chloroquine should be considered comparable to HCQ.
Brief History

Before hydroxychloroquine, in many years before, was the compound quinine. Quinine is a quinidine alkaloid, meaning its structure contains a few cyclic rings containing nitrogen that provide the alkaline nature to the compound.

The history of quinine’s usage spans several centuries, with some indications of its use being documented going back over 400 years, which truly highlights the long history of natural remedies used by many of our ancestors.
Here’s an excerpt from Achan et. al. 2011 alluding to the lore behind quinine usage:
Quinine, as a component of the bark of the cinchona (quina-quina) tree, was used to treat malaria from as early as the 1600s, when it was referred to as the "Jesuits' bark," "cardinal's bark," or "sacred bark." These names stem from its use in 1630 by Jesuit missionaries in South America, though a legend suggests earlier use by the native population[2]. According to this legend, an Indian with a high fever was lost in an Andean jungle. Thirsty, he drank from a pool of stagnant water and found that it tasted bitter. Realizing that the water had been contaminated by the surrounding quina-quina trees he thought he was poisoned. Surprisingly, his fever soon abated, and he shared this accidental discovery with fellow villagers, who thereafter used extracts from the quina-quina bark to treat fever [3]. The legend of quinine's discovery accepted in Europe differs though, and involves the Spanish Countess of Chinchon who, while in Peru, contracted a fever that was cured by the bark of a tree. Returning to Spain with the bark, she introduced quinine to Europe in 1638 and, in 1742, botanist Carl Linnaeus called the tree "Cinchona" in her honour [4].
As the story goes, the antimalarial effects of quinine are derived from the bark of the cinchona tree, and was used to make beverages and consumed for the therapeutic benefits. It wasn’t until the early 1800s when quinine was purified and isolated from the bark by scientists Pierre-Joseph Pelletier and Joseph Caventou, allowing it to be administered more broadly. Even with all of its benefits, there were many concerns with quinine’s toxicity, although the drug would see widespread usage for many decades.
As science in the field progressed towards synthetic compounds, German scientists working for Bayer would eventually come across the compound chloroquine in 1934, although concerns about its toxicity shelved the compound for nearly a decade. Note that even though it shares a similar name to quinine the structure is very different, consisting of an aminoquinoline instead of a quinidine structure.
It wouldn’t be until World War II that chloroquine began to see large-scale usage.
Here’s an excerpt from Njaria et. al. 2015 describing the scenario:
Despite exhibiting potent antiplasmodial activity, this compound was initially neglected for almost a decade due to toxicity concerns in humans. However, during World War II, the US government sponsored clinical trials that demonstrated the therapeutic value of chloroquine (CQ) as an antimalarial and its superiority over existing drugs, thereby heralding its widespread use in the treatment and prevention of different forms of malaria [2,3].
And it was from this widespread use of prophylactic chloroquine during WWII that led to the discovery of its immunomodulatory effects.
Taken from Ben-Vzi et. al. 2012:
During the Second World War, millions of soldiers took antimalarial prophylaxis, and the observation that antimalarial improved the soldiers’ rashes and inflammatory arthritis led to the first trial that showed the efficacy of antimalarials in systemic lupus erythematosus (SLE) [4]. Since then, the role of antimalarials in rheumatic diseases was established and today its use is widespread in SLE and in rheumatoid arthritis (RA) [5–7].
Even still, the toxicity profile of chloroquine was an area of concern, although it began to see widespread usage both as an antimalarial as well as an immunomodulator against systemic lupus and rheumatoid arthritis.
Fortunately, nearly a decade (~1955) after chloroquine’s widespread usage a new derivative was created which added a hydroxyl group (-OH) to the structure and helped reduce the toxicity of chloroquine by nearly a third. Of course, this compound (with the additional hydroxyl group) is named Hydroxychloroquine (AKA Plaquenil).
Although Chloroquine still sees some usage in modern times, Hydroxychloroquine has been adopted as one of the most widely used antimalarials and immunomodulators out there. In fact, its status as one of the most widely used antimalarials garnered it the moniker of an “essential medicine”, according to the W.H.O.
Therapeutic Uses
As we have outlined above, Hydroxychloroquine has been used predominately as an antimalarial and immunomodulator. However, over the years plenty of other possible uses have been discovered, although not all of them have been fully realized for large-scale human use.
Here, I’ll mainly outline the antiviral and immunomodulatory mechanisms of action of HCQ and indicate how this plays a role against SARS-COV2 infection. I’ll also indicate other possible uses, although this area has not been as extensively researched so it will only be a cursory glance.
Antimicrobial Activity
HCQ exhibits several antimicrobial mechanisms, mostly by hindering the endocytic pathway and altering how cells intake exogenous substances. HCQ’s weakly basic nature causes a cascade of events, such as the inhibition of viral binding to host cells which prevents pathogenic uptake. One of the main targets of HCQ are lysosomes, which help with the metabolism of cellular compounds through acidic degradation which are then exported to be expelled or presented on a cell’s surface.
In the case of SARS-COV2, one of the hypotheses is that HCQ may prevent glycosylation of the ACE-II receptor due to lysosomal inhibition, and thus viral binding would become inhibited, although there are a few other possible mechanisms as well (as outlined in the figure below).

Immunomodulation
Inhibition of the endolysosomal pathway doesn’t just provide antimicrobial properties, but also helps to regulate autoimmune disorders. By inhibiting the activity of lysosomes, the presentation of MHC-Class II autoantigens (antigens that cause a person’s own immune system to illicit a response against itself) is hindered and therefore would not be targeted for cell death.
One of the other possible targets are toll-like receptors (TLR) which are responsible for activating the innate immune system and producing a pro-inflammatory response. In autoimmune disorders, the release of cellular debris may lead to activation of the TLR pathway and produce the inflammatory response seen in diseases such as lupus and rheumatoid arthritis.
Once again, HCQ may prevent both antigen presentation and antigenic binding, both of which may play a hand in the inflammatory response.
In later SARS-COV2 disease progression viral replication is largely replaced with an over reactive immune response that leads to a cytokine storm and systemic inflammation. Here, administration of HCQ was thought to quell the production of cytokines in a similar manner to that seen in autoimmune disorders. Unfortunately, there is a lot of controversy surrounding administration of HCQ in this stage, and possible cardiac arrhythmias and prolonged QT intervals from adverse reactions have caused the medical field to question HCQ’s usage against COVID.

Other Therapeutic Uses
HCQ has been indicated to have many other therapeutic uses. Although they won’t be outlined in detail here (as they have not been fully researched to the same extent as the antimicrobial and immunomodulatory actions) I’ll provide a brief overview. Note that most of this information will be derived from these following papers:
Diabetes: HCQ seems to have a hypoglycemic effect, and studies indicate its administration, along with insulin, may lead to a reduction in glycated hemoglobin levels. Although there may be some benefits to using HCQ for diabetes militus, current treatments seem to be effective so there may be no reason for its use for diabetes.
Cardioprotection: You would think a drug that has been demonized for possible cardiotoxicity would not have a protective effect on the heart, yet there are some studies that suggest HCQ may be cardioprotective. People diagnosed with rheumatoid arthritis tend to suffer from cardiac complications due to the disease, medications, or other comorbidities. HCQ seems to reduce lipid biomarkers (cholesterol, LDL, and triglyceride levels) in those suffering from RA, suggesting possible protective benefits against adverse cardiovascular events.
Antithrombotic: HCQ and other chloroquine derivatives seem to hinder platelet aggregation and reduce thrombus formation, indicating possible usage for diseases such as antiphospholipid syndrome (APS), although the mechanisms have not been fully elucidated.
Anticancer: The increased permeability of lysosomes by HCQ may sensitize them to cancer treatments such as radiotherapy and chemotherapy, thereby providing a possible anticancer mechanism of action. Radiotherapy may become more effective due to increased cancer cell membrane permeability, while chemotherapeutics may be blocked from being exported by cancer cells and thus a buildup of a therapeutic may increase its potency.
Adverse Effects
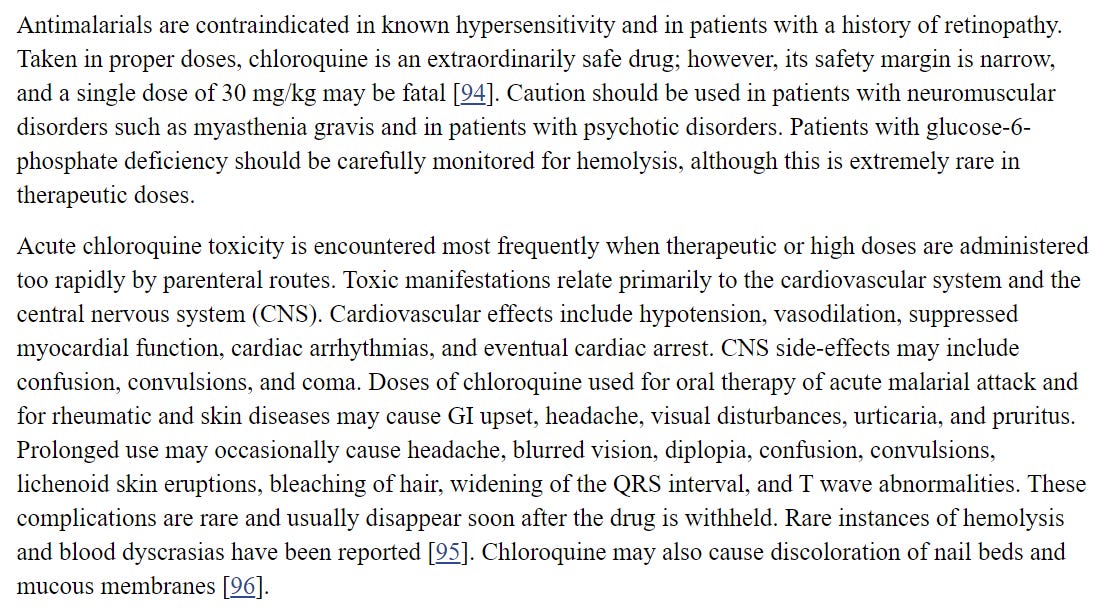
At the typical doses HCQ tends to be relatively safe and there tends to be no severe adverse events. Nonetheless, in higher doses or in certain groups with other comorbidities, retinopathy and cardiotoxicity may occur.
Here’s a general idea of possible adverse events, although note that there are many underlying reasons such events may become present.
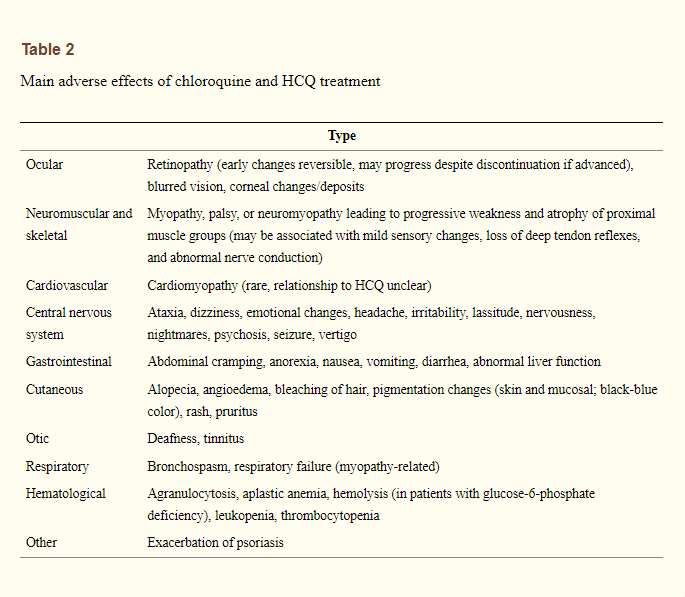
As indicated in an excerpt from Ben-Zvi et. al. 2012:
Hydroxychloroquine as a Multifaceted Drug
The use of Quinine and Chloroquine derivatives span many decades, providing a window into the long, well-established history of these antimalarial drugs. Not only does Hydroxychloroquine exhibit antimicrobial and immunomodulatory effects, it may also be used for other diseases such as metabolic disorders and cancer.
The broad-spectrum activity of HCQ indicates why it was seen as a potential candidate against SARS-COV2, and its widespread accessibility would make it an outstanding candidate against the virus. As we will see in my next post, the data around HCQ and SARS-COV2 is very murky, and would require some investigating.
Thank you for reading my newsletter. If you enjoy my articles please consider becoming a free subscriber in order to receive notifications.
And share with others who may find these newsletters interesting.
Also, please consider becoming a paid member. The research and work put into these articles takes many hours and being a paid subscriber allows me to continue to do this full time.
Citations:
Mehra et. al. 2020. Retraction—Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7274621/
Schrezenmeier et. al. 2020. Mechanisms of action of hydroxychloroquine and chloroquine: implications for rheumatology. Taken from https://www.nature.com/articles/s41584-020-0372-x
Achan et. al. 2011. Quinine, an old anti-malarial drug in a modern world: role in the treatment of malaria. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3121651/
Njaria et. al. 2015. Chloroquine-containing compounds: a patent review (2010 – 2014). Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7103710/
Ben-Zvi et. al. 2012. Hydroxychloroquine: From Malaria to Autoimmunity. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7091063/
Faraone et. al. 2020. Recent Clinical and Preclinical Studies of Hydroxychloroquine on RNA Viruses and Chronic Diseases: A Systematic Review. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7696151/
Kalia et. al. 2007. New concepts in antimalarial use and mode of action in dermatology. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7163426/



"Chloroquine is a potent inhibitor of SARS coronavirus infection and spread" -- 2005:
https://pubmed.ncbi.nlm.nih.gov/16115318/
Very informative!
Many decades ago an article like this one, explaining to non-scientists how HCQ works would appear in a respected publication like NYT.
Our world would have been very different if MSM was doing actual journalism.
Thankfully now we have writers like you and hopefully more people discover your substack.