Growing recognition of long-term COVID vaccination adverse reactions
Part I: Looking into small fiber neuropathy related to COVID and the vaccines.
Initially a look into a widely circulated Science article, this post has branched into looking at the two complications outlined in the article and diving into relevant literature. Part I here looks at small fiber neuropathy. The second will look at case reports of POTS and possible explanations for these adverse reactions.
Correction 7.11.2023: In the Mastropaolo, M., & Hasbani, M. J. case report I mentioned that prior history of SARS-COV2 appeared negative by way of a negative antinuclear antibody test. However, I unfortunately conflated antinuclear with antinucleocapsid. Antinuclear antibodies are a measure for autoantibodies which may attack the nucleus of cells, and thus are distinct from nucleocapsid proteins found in SARS-COV2. The sentence making this improper conflation has been removed, and readers should instead consider that no evidence of prior infection history was provided by the authors.
Also, a table for Schelke, et al. noting elevated adrenergic autoantibodies has also been included.
Within the past week several Substacks have covered a rather telling article published in Science, which has made the discussion of long-term vaccine injuries more palatable to a mainstream audience.
As stated, several people have already covered this article before, including Igor Chudov and Stephanie Brail of Wholistic.
The article follows after a January 2022 Science article which made note of this possibility of “Long vax”. It’s an article I’ve mentioned before when discussing Long COVID, and unlike the recent article published last week the January 2022 one heavily downplays these adverse reactions.
Note that the use of “Long vax” may actually be improper when compared to Long COVID unless the actual timeframe is considered for these patients. The weeks following a COVID infection are considered to be the acute phase of the illness, with weeks-months afterward being considered the post-acute phase i.e. the Long COVID phase of illness. Therefore, when describing “Long vax” a consistency in terminology would suggest that we are referring to symptoms that persist after the post-acute phase of vaccination.
There’s quite a few interesting nuggets in this article, including the admittance by some doctors that they are seeing more people coming into the clinic describing these post-vaccine symptoms that are more than just coincidental:
But in recent months, what some call Long Vax has gained wider acceptance among doctors and scientists, and some are now working to better understand and treat its symptoms.
“You see one or two patients and you wonder if it’s a coincidence,” says Anne Louise Oaklander, a neurologist and researcher at Harvard Medical School. “But by the time you’ve seen 10, 20,” she continues, trailing off. “Where there’s smoke, there’s fire.”
On cardiologist Harlan Krumholz, who raised concerns that post-vaccine injuries would be seized upon by “antivaxxers”, eventually allowed for the inclusion of post-vaccine injured individuals into a study that focused on Long COVID patients.
Krumholz makes the following remark:
“I’m persuaded that there’s something going on” with these side effects, Krumholz says. “It’s my obligation, if I truly am a scientist, to have an open mind and learn if there’s something that can be done.”
There’s also this rather revealing remark about the January 2022 article, in which the article had led to many people reaching out and discussing their post-vaccine symptoms:
SCIENCE FIRST wrote about these health concerns in January 2022, describing efforts by scientists at the National Institutes of Health to study and treat affected individuals. A study including 23 people was posted as a preprint in May 2022 but never published. Following Science’s story, almost 200 people contacted the journal sharing their postvaccination symptoms.
This is rather striking, because it alludes to the fact that the downplaying and suppression of any vaccine adverse reaction discussion likely had some influence on the number of adverse events that get reported, with people wrongly assuming that any symptom they may have post-vaccination is likely attributed to some other factor.
If the mainstream press was more open, there’s a greater possibility that many more people would have come forth with their stories of post-vaccine injuries. It’s truly telling that these discussions are only becoming more widely discussed 2 years after the vaccine rollout.
I recommend that people read the article in full as it’s a rather short one.
For me, the main point worth addressing are the two post-vaccine complications described in the article: small fiber neuropathy and postural orthostatic tachycardia syndrome, or POTS.
As people continue to search for answers in why these adverse reactions are occurring in certain individuals, it’s necessary to examine these complications and consider what mechanisms may be occurring.
Small Fiber Neuropathy Overview
The first complication discussed in the Science article is called small fiber neuropathy1.
This disease is associated with two nerve fibers in particular, Aδ (Delta) fibers and C fibers. Unlike Aα (Alpha)- and Aβ (Beta)-fibers, Aδ and C nerve fibers are smaller in diameter, partially due to the lack of myelination (Aδ fibers are partially myelinated whereas C fibers are not myelinated at all) as well as actual nerve fiber size, which is where the term “small fiber” comes from.
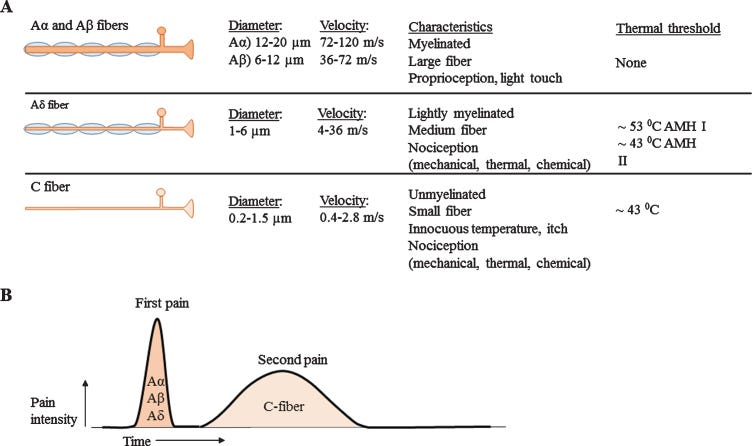
These small fibers are generally found within the peripheral nervous system, dictating somatic (sensory) and muscle functions, as well as autonomic functions. These are the nerves partially responsible for the sensation of pain and heat, as Aδ fibers contribute to the sharp tingling, prickling sensation one feels while C fibers produce a longer, burning sensation, as outlined in the Raasing, et al.2 figure above.
Dysfunction and deterioration of these fibers can lead to small fiber neuropathy, which can feel like shocks, tingles, and burning within the extremities of the bodies such as hands and feet.
Cascio MA, & Mukhdomi T. provide a more comprehensive explanation for some of these symptoms of SFN:
Patients with SFN often present initially with neuropathic foot pain. Symptoms may be mild at onset, with some patients noting a vague discomfort in the feet. Reported descriptions may include numbness in the toes, a wooden quality in the feet, or a feeling that the patient describes as walking on sand, golf balls, or pebbles. Burning pain in the feet expending proximally in a stocking-glove distribution is often the most bothersome and typical symptom.
This burning is often accompanied by aching or stabbing pains, pins and needles sensation, electric shock, or cramping in the feet and calves. Patients with SFN typically experience the worst of their symptoms at night, often complaining of restless legs, bed sheet intolerance, and clothes causing allodynia or dysesthesia. Some patients do not report pain but note a feeling of swelling and tightness in their feet. Autonomic fiber involvement may lead to additional symptoms, including dry mouth, dry eyes, constipation, bladder incontinence, orthostatic dizziness, sexual dysfunction, red or white skin discoloration, or trouble sweating.
Stocking-glove distribution sounds a bit confusing, but it refers to the fact that these symptoms present predominately within the hands and feet (alluding to stockings for feet and gloves for hands). Symptoms that usually start within the extremities, especially the feet, that make their way towards the center of the body are described as length -dependent SFN. More diffuse symptoms of SFN are thus described as being non-length dependent.
Note that the above symptoms are somatic-related. Autonomic manifestations of SFN may include fatigue, headaches, other changes in cognition, and even alterations in cardiovascular function.
Because small fibers lack myelination, it’s argued that demyelination may not provide a pathogenic explanation for small fiber neuropathy unless other, more heavily myelinated neurons are also targeted.
Thus, when viewing vaccine-related neurological complications it’s important that the actual nerves being targeted be characterized and described to differentiate possible demyelination processes.
Causes for SFN are extremely broad, with early suggestions of this disease pointing towards viral infections. Neurotoxins, drugs, genetics, immune-mediated, and even low vitamin B12 may be associated with SFN. It may also be diagnosed as being idiopathic in nature, suggesting that the actual causes for SFN are unknown for the specific patient. Some vaccines have been associated with presentation of SFN as well.
Diagnosis of SFN may rely on skin biopsies taken from various parts of the body including above the ankle, above the knee, and below the hip, which at first sounds rather strange. However, as mentioned in a Cleveland Clinic article, the low conductivity of these small nerves means that their activities may not be properly captured in nerve conduction studies, and so examination for damages to nerves via skin biopsies may help in the diagnosis of SFN.
It’s important to make note of the use of skin biopsies, as several case reports of SFN related to SARS-COV2 and vaccination examine skin biopsies of patients.
Additional methods for discerning SFN may also rely on pricks and heat to see if patients notice any of these sensations (lack of sensation suggesting possible SFN).
COVID Infection and Vaccine-related SFN
As alluded to in the Science article, several reports of SFN have been documented associated with both COVID infection as well as the vaccines.
A study from Abrams, et al.3 noted neuropathy in a small subset of COVID patients with varying degrees of illness (some were mild or asymptomatic). The time of symptom presentation ranged from 2 weeks to 2 months post-infection, with only one patient appearing to show signs of paresthesia (abnormal skin sensations) during infection. Several of the patients confirmed to have SFN by skin biopsies noted a length-dependent presentation of SFN by differences in knee skin biopsy results compared to the thigh.
This appears to be a rather well-cited article, and notes that the manifestation of SFN may not be related to infection severity.
Cases of vaccine-related SFN have been reported as well:
A case report from Waheed, et al.4 mentions a 57-year old woman who presented to the clinic 1 week after receiving a second dose of the Pfizer/BioNTech vaccine, with reported symptoms of dysesthesias (unusual or painful touch sensations) in the feet which spread to the calves and partially presented in her hands.
There is no evidence of prior SARS-COV2, and no indication of symptoms after the first dose of the vaccine. Skin biopsies confirmed SFN due to lack of nerves, with no noticeable histological changes noted. The patient was provided the anticonvulsive Gabapentin and showed a near-full resolution of symptoms in the following weeks, although the patient appeared to still experience stocking-type small fiber modality loss at the time of follow-up.

From Waheed, et al. Skin biopsies from the foot, calf, and thigh were suggestive of SFN due to lack of staining via protein gene product 9.5 antibodies. Protein gene product 9.5 is a cytoplasmic protein produced by neurons, and so lack of staining would suggest loss of these neurons. No abnormal histology was reported in these biopsies.
A case report from Schelke, et al.5 noted a 52-year old man man who began experiencing paresthesia along with a burning/stabbing pain within his hands, feet, and eyes which were accompanied with tinnitus within the right ear. His symptoms worsened into orthostatic dysregulation/POTS within the following months, to the point that he could not stand or walk without experiencing syncope (fainting).
Lab tests revealed elevated antibody titers against adrenergic receptors including ACEII, suggesting a possible autoantibody-mediated neuropathy.
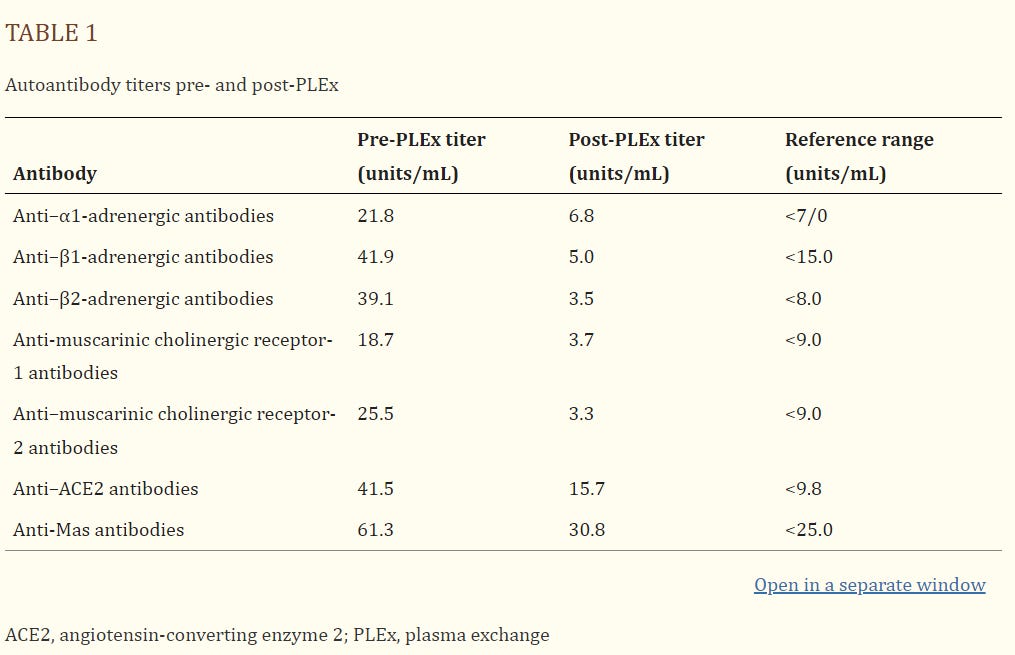
From Schelke, et al. Table 1. Comparisons of autoantibody titers before and after plasma exchange treatment. Note the column on the rightmost side which explains typical ranges in healthy individuals. The patient was provided various medications including Nadolol (antihypertensive) for his tachycardia, Gabapentin, Amitriptyline and Trazodone (antidepressants/nerve pain medications) with limited success.
Edit 7.11.2023: Please note that the Nadolol appeared to help with the tachycardia. However, the other treatments didn’t appear to be effective with the management of neuropathy.
Treatment with Intravenous Immunoglobulins were halted after the second course due to anemia. Subcutaneous Immunoglobulins appeared to improve pain symptoms but worsened the tinnitus.
Patient improvement appeared to occur after several rounds of plasma exchange (PLEX)- 5 rounds over the course of 10 days. The patient’s symptoms improved and several fully resolved, along with apparent reductions in autoantibody titers.
In addition, a case report from Mastropaolo, M., & Hasbani, M. J.6 noted a 39-year old man who presented with left deltoid pain, which followed with left arm pain and numbness days after receiving the first dose of the Pfizer/BioNTech vaccine. The numbness and tingling began to spread to other parts of the body in the following weeks, which also came with burning dysesthesias within his extremities.
Interestingly, the patient showed extremely high antibody titers against Fibroblast growth factor receptor 3 (FGFR3). These receptors are critical for various cellular functions, and have been associated with some cases of SFN, again suggesting a possible autoimmune-related association for these post-vaccine symptoms. These findings led to several courses of IVIG as a treatment.
Skin biopsies of the left foot and calf noted abnormalities in staining (lack of PGP9.5 staining similar to that of Schelke, et al.) at 148 days post-vaccination. A skin biopsy taken at 405 days post-vaccination and after IVIG treatment notes formation of epidermal neurites (arrows).

Towards Consilience
Remember that the intent of looking into these case reports is to find evidence of consistency in pathology.
The main question of autoimmunity post-vaccination will be saved for the next post, however in this case it’s worth highlighting that two of the case reports above make note of autoantibody titers. Schelke, et al. looked at anti-RAAS antibodies. Although this is only one case report, it raises an interesting question of anti-ACEII antibody formation from either COVID infection or vaccination.
If such an event is rather widespread, it provides a hypothesis that doesn’t require the assertion of forever spike. There’s no indication for how long spike actually persists in the body of those who are vaccinated, but such an autoimmune response would suggest that there would be no need for continuous spike- the immune system can target ACEII receptors on their own by way of autoimmunity. Again, this will be explored a little bit further in the following post.
With respect to the anti-FGFR3 antibodies noted in Mastropaolo, M., & Hasbani, M. J.’s case report, these antibodies do appear to be associated with various neuropathies. Mutations in FGFR37 have also been associated with a host of different diseases, including various cancers (FGFR3 appears to associate with bladder cancer). It’s a bit of a stretch to argue that lack of FGFR3 functionality may be associated with cancer. Rather, it’s more important to consider the effects of FGFR3 loss within the greater context of disease.
Given that both of these case reports appear to have looked at different autoantibodies and came out with positive results may, again, point to a possible role of autoimmunity in all of these adverse reactions.
However, the difference in examination and treatment also suggests that there is a lack of consistency in the literature when evaluating a patient for SFN. This lack of consistency means that a lot of otherwise critical information may be missed in these case reports. For instance, does the individual in the Schelke, et al. case report also have higher anti-FGFR3 antibody levels? Does the individual in the Mastropaolo, M., & Hasbani, M. case report also have autoantibodies that target adrenergic and ACEII receptors?
There’s still a lot that continues to be missing from these case reports.
This article has gone on somewhat of a tangent, in which I took a look at what SFN is and what some of the literature suggests about this complication. As for the Science article, it’s rather interesting that such an article has come out years after the vaccine rollout.
It raises a question of why these sorts of articles did not come out earlier and why the topic of adverse reactions did not receive more mainstream coverage outside of remarks made towards myocarditis.
Hopefully articles such as the Science one allows for greater discussion of adverse reactions, and hopefully more people will feel open to coming out and sharing their stories so that more attention can be brought to the harms that these vaccines have caused.
Anyways, the next post will look a bit into POTS, and dive a bit deeper into the autoimmunity argument.
Substack is my main source of income and all support helps to support me in my daily life. If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists such as myself to provide work outside of the mainstream narrative.

Cascio MA, Mukhdomi T. Small Fiber Neuropathy. [Updated 2022 Dec 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK582147/
Raasing, L. R. M., Vogels, O. J. M., Veltkamp, M., van Swol, C. F. P., & Grutters, J. C. (2021). Current View of Diagnosing Small Fiber Neuropathy. Journal of neuromuscular diseases, 8(2), 185–207. https://doi.org/10.3233/JND-200490
Abrams, RMC, Simpson, DM, Navis, A, Jette, N, Zhou, L, Shin, SC. Small fiber neuropathy associated with SARS-CoV-2 infection. Muscle & Nerve. 2022; 65( 4): 440- 443. doi:10.1002/mus.27458
Waheed, W., Carey, M. E., Tandan, S. R., & Tandan, R. (2021). Post COVID-19 vaccine small fiber neuropathy. Muscle & nerve, 64(1), E1–E2. https://doi.org/10.1002/mus.27251
Schelke, M. W., Barcavage, S., Lampshire, E., & Brannagan, T. H., 3rd (2022). Post-COVID-19 vaccine small-fiber neuropathy and tinnitus treated with plasma exchange. Muscle & nerve, 66(4), E21–E23. https://doi.org/10.1002/mus.27696
Mastropaolo, M., & Hasbani, M. J. (2023). Small Fiber Neuropathy Triggered by COVID-19 Vaccination: Association with FGFR3 Autoantibodies and Improvement during Intravenous Immunoglobulin Treatment. Case reports in neurology, 15(1), 6–10. https://doi.org/10.1159/000528566
Krook, M.A., Reeser, J.W., Ernst, G. et al. Fibroblast growth factor receptors in cancer: genetic alterations, diagnostics, therapeutic targets and mechanisms of resistance. Br J Cancer 124, 880–892 (2021). https://doi.org/10.1038/s41416-020-01157-0








What is being described is what I expected to see due to "borrowed" gp120 envelope glycoproteins. Thanks Ralph.
The Molecular and Pharmacological Mechanisms of HIV-Related Neuropathic Pain (2013)
...The most common complaint of HIV-DSP is pain on the soles; the pain is typically bilateral, of gradual onset, and described as ‘aching’, ‘painful numbness’, or ‘burning’[34]. Patients often have hyperalgesia and allodynia in a stocking and/or glove distribution. The feet are tender to touch, wearing shoes is painful, and the gait becomes ‘antalgic’. In a typical length-dependent fashion, the dysesthesias ascend proximally up the lower extremities over months, and may begin to involve the fingertips at around the same time as they reach the mid-leg level [33, 35]. It is usually most severe on the soles of the feet, and is typically worse at night.
Pathologically, the most common histological feature of both DSP and ATN is characterized by loss of DRG sensory neurons, Wallerian degeneration of the long axons in distal regions, DRG infiltration by HIV-infected macrophages, and a 'dying back' sensory neuropathy [36-40]. Early on, small, unmyelinated sensory fibers are lost, with eventual destruction of the large myelinated fibers as the disease progresses in the patients with HIV. In the periphery and the DRG, there is infiltration of macrophages and other inflammatory cytokines [41]. Clinically, these two forms (HIV-DSP and ATN) of HIV sensory neuropathies are difficult to distinguish.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3763758/
Perchance, did any of these studies offer treatment ideas?