Everyone is Getting COVID. It’s time to learn and deal with the virus.
PART II: At-Home Remedies in an Omicron-Riddled World
Therapeutics in an Omicron World
This will serve as the meat for the rest of this post. There will be plenty of topics or treatments that I have previously covered that will overlap with Omicron. After all, we should expect a good deal of overlap considering that Omicron is still a beta coronavirus and therefore many of our prior topics will still hold up here. Because of this I won’t go over supplements such as Vitamin D3 or Quercetin, which are not likely to change in dynamics with COVID. In fact, supplements should be examined for their effects not just on COVID but for overall health benefits, especially in those who are likely to already have vitamin deficiencies.
For more information on vitamins and supplements, I’ll refer you all to Robin Whittle’s Substack Nutrition Matters for his posts on Vitamin D3, as well as Heather’s post from several months prior. I also have my Quercetin Anthology Series as well, which drew many of you to this Substack in the first place. There are several places to read about supplementations and overall they are all likely to hold up in principle against Omicron.
With that being said, there will be a few early, at-home treatments which may prove to be more effective due to the different dynamics of Omicron and so we will focus mostly on those.
Before we begin, I’ll remind everyone about some of the new dynamics with Omicron and why certain treatments may play bigger roles than before:
Omicron appears to dominate in the upper respiratory tract. Several of the studies we have looked at have indicated that Omicron infection leads to a much higher viral load in the nasal passageway compared to Delta and even Wildtype COVID. This provides us with better, more direct routes of targeting COVID with items aside from orally ingested drugs as therapeutics that may directly target the nose or throat may target a large level of viral load.
Omicron’s infection appears to rely more on cell-to-cell viral transfer, likely through the use of the endosomal pathway. Certain drugs elicit their antiviral properties through direct targeting of the virus to prevent it from replication and spreading. However, some drugs may target vital host pathways that the virus utilizes and inhibits viral replication through a more indirect route. If Omicron goes through the endosomal pathway to a greater degree than prior variants, it would make sense that drugs that alter the functionality of the endosomal pathway will be even more effective against Omicron. For that reason, I’ll briefly discuss 2 drugs of choice, and they’re likely ones you have heard of before.
Monoclonal Antibodies Pulled by the FDA
I’ll first start off with a few remarks about monoclonal antibodies.
A few days ago the FDA made a decision to remove the EUAs for two widely used monoclonal antibody treatments; Regeneron and Eli Lilly’s monoclonals.
I have written extensively on why these two were the most likely to lose effectiveness while Sotrovimab appears to hold up against Omicron in my Omicron/Monoclonal Anthology Series.
However, I also made it clear that a rash removal of these monoclonals may prove harmful if common sense and rational thinking are not used to decipher which monoclonal antibody should be used for which patient.
The evidence so far is pretty clear that Omicron is far less severe than Delta, and so even if we have lost 2/3rds of our available arsenal of monoclonals, we may not be as dependent on them for treatment if many people get mild illness. However, not everyone will experience just mild illness, and there is still a chance that there may be some Delta still in circulation among the population.
Not only that, but include the fact that the CDC does not have a good track record with their COVID surveillance and it’s easy to see how we may be running into a dangerous situation.
As I previously stated, an easy differential diagnosis for Omicron would be to look for an “S Gene Drop” when conducting PCR. It’s a heuristic-based approach, but it may still provide some benefit to examine which genes were amplified in order to see if a patient may indeed be infected with a different variant.
Hopefully Omicron will provide us with less of a need to depend on monoclonal antibodies, but it still may lead to precarious scenarios where the absence of any treatment may prove to be even worse than having ones that are ineffective. This is something we have witnessed all throughout the pandemic, and we’ll emphasize this point even more here further on in the post.
Nasal and Oral Remedies
Omicron’s apparent higher level of viral load within nasal epithelial and throat means that therapeutics that target the nose and throat may be even more beneficial in clearing away the virus.
Unfortunately, the arena surrounding at-home therapeutics still continues to be spotty. The research doesn’t appear to have changed much since I last checked. Pair that with many strange attacks by the media against the use of at-home remedies and we can see that this whole area is nothing but a hot mess.
Because of this, I will point you all to my post on at-home nasal remedies and examine some of the items mentioned there as they will be reiterated to an extent here. For those who would like an additional quick review of viricidal gargles and nasal sprays, check out this review paper by Kramer et. al. It even includes different techniques from different countries around the globe and may be something worth looking at for a brief overview. It’s interesting that there are a few countries that have adopted prophylactic and early exposure nasal/oral remedies since nothing of the sort seems to be happening here in the US.
A Brief Correction to a Prior Study
With that being said, I do need to add some clarity to one of the studies I cited. In my post, I mentioned this study by Guenezan et. al. in which the researchers found that not only did Povidone-Iodine not reduce the days of COVID infection, but in fact nearly 42% of those in the experimental group experienced hyperthyroidism.
What should be pointed out here is that the methodology outlined by the researchers are, to be frank, extremely excessive in their Iodine usage (emphasis mine):
Intervention consisted of 4 successive mouthwashes and gargles with 25 mL of 1% aqueous PI solution each (Mylan, Merignac, France), followed by one 2.5-mL nasal pulverization of the same solution into each nostril using an intranasal mucosal atomization device (MAD Nasal, Teleflex, Morrisville, North Carolina) connected to a 5-mL syringe while sniffing and 1 application on each nasal mucosa of a dab of 10% PI ointment followed by a massage of the nostril to help spread the ointment. Patients were trained during the first decolonization session, and received the necessary materials and a guide to help them perform the following sessions 4 times a day for 5 days.
Although the high usage of PI did not seem to significantly reduce days of infection, we can see that this methodology can be considered highly excessive. It’s no wonder that so many patients within the treatment group had hyperthyroidism, and it highlights the importance of examining the methodology of experiments and comparing them to real-life scenarios for their feasibility in common, everyday usage. This study itself should not be used as a reflection of Povidone-Iodine’s lack of effectiveness but to highlight that, like with all things, there is a point where anything can become toxic and care should be taken to avoid such a point.
Examining Oral & Nasal Remedies
To turn back to the main point, many at-home therapeutics fall into two categories; mechanical or chemical. Mechanical is straightforward and usually refers to techniques or remedies that are intended to irrigate or flush nasal or oral passages. Many mechanical techniques tend to be paired with chemicals, but the main purpose of mechanical techniques are to quickly eliminate viral particles through physically removing them rather than through their inactivation or breakdown from chemical reactions.
The most common mechanical method is the use of a neti pot, which are small pots that are usually filled with a saline solution or sometimes with other compounds such as very dilute essential oils or Povidone-Iodine, and are then poured into one nostril at an angle and allowed to flush and drain out the other nostril.
Nasal sprays may also fall under this category, although they are far less effective at flushing or irrigating, although there are many types of nasal sprays available including ones that contain viricidal properties. However, it should be noted that many nasal spray viricidal have not been tested on SARS-COV2, although correlations can be drawn based on their effectiveness against other viruses.
For the mouth, the most typical mechanical technique is gargling, and similar to the use of a neti pot many gargling solutions can be as simple as a saline solution to very dilute compounds such as hydrogen peroxide, Povidone-Iodine, or even everyday ethanol-based mouthwashes.
These type of techniques have come under heavy scrutiny as a heavily ineffective manner of dealing with COVID, and some websites have even commented that these are not intended to be used to prevent COVID. The neti pot link above makes the same argument, although it links to a WHO site which doesn’t appear to make any mention of neti pot usage, and in fact I have a lot of skepticism with the information presented on that page.
Many of these techniques aren’t used to eliminate viral particles, but instead are used for every day issues such as seasonal allergies or congestion. For gargling, millions of people use mouthwash daily as part of their dental routine. There are plenty of daily uses for these techniques irrespective of whether or not they’re intended to eliminate COVID, so the rampant attacks about using such techniques are rather infuriating because of that factor alone.
But let’s say that people do intend to use it for COVID. Again, under such circumstances many of these techniques would sever as dual purpose. Maybe neti pots don’t remove COVID (although I have posted a study that says otherwise below), but they would still help with congestion caused by COVID. Or even mouthwash, which may not eliminate COVID but will help to freshen your breath and reduce gingivitis regardless. Under most circumstances, there’s very little risk to deploying these techniques and even if there is no reward the lack of harm shouldn’t preclude people from making an attempt to try some of these methods.
(I would like to point out that this information is intended to be purely informative and not to be used as an instructional guide!)
There’s a lot more to say on this front, but in general it’s quite alarming to see the amount of attacks aimed against even attempting to try rather harmless methods to try to protect or eliminate the virus.
Just a Few Studies
Even though the research is lacking in this arena, I’ll cite a few general studies that examined a few at-home remedies.
Although the evidence is scarce on the effectiveness of neti pots, there is a recent paper that began circulating online that indicated those who used neti pots for nasal irrigation were 8 times less likely to be hospitalized for COVID.
In this study by Baxter et. al. researchers assigned COVID positive patients to use neti pots for nasal irrigation twice a day for 14 days. Patients were either told to use saline solution with Povidone-Iodine or saline solution with sodium bicarbonate (baking soda).
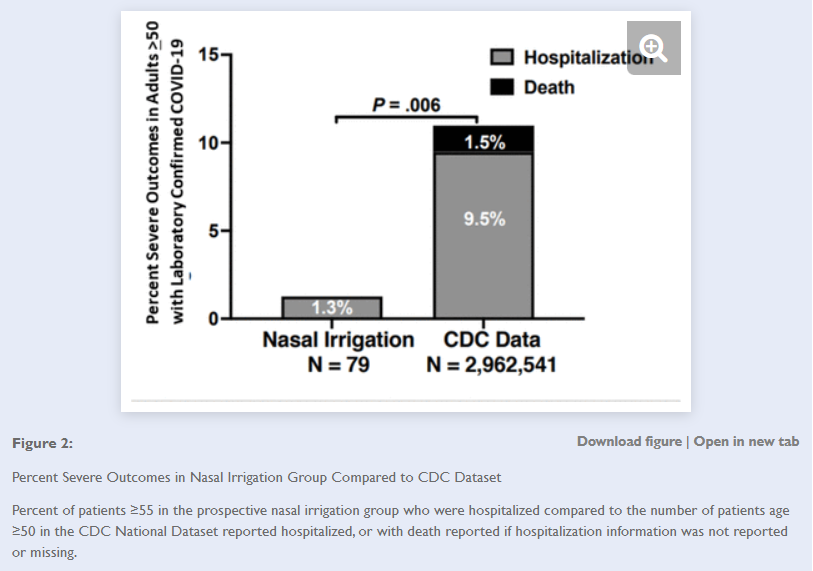
What’s shocking here is that the researchers suggest that implementation of neti pot usage among the elderly were likely to have reduced the number of hospitalized elderly patients by over 1 million! Granted, some skepticism should be taken when making such a comparison considering that such a comparison are likely to be affected by plenty of bias. There’s also no way to directly correlate the results from these researchers studies to the national average, and drawing such parallels should be met with skepticism. Nonetheless, the results here are quite startling in their possible implications.
Our results support that pressurized nasal irrigation reduces the likelihood of hospitalization in high-risk COVID-19 + patients, suggesting a safe and over the counter measure with potentially vital public health impact. Nationally, the reduction from 11% to 1.3% as of November 2021 would have corresponded in absolute terms to over 1,000,000 fewer older patients requiring admission. While one study found 47% of those 50 and older had continued symptoms 14 – 21 days after diagnoses,16,17 only 13% in our study had symptoms at day 14. If confirmed in other studies, the potential reduction in morbidity and mortality worldwide could be profound.
Whether or not neti pots are actually effective at reducing hospitalization rates, there’s not doubt that implementing them during an infection is likely to help with congestion, especially considering that congestion is a very common symptom with Omicron.
In one pilot, open-labeled, randomized study by Mohamed et. al. researchers placed patients who are within early stages of COVID (note that they did not even present with fevers of respiratory symptoms yet) into one of 4 test groups. In total 20 patients were examined (5 per group), so it’s important to note that this was a pilot study that utilized a very small sample group, and therefore the results of this study should be examined with a good deal of skepticism. Also, I should point out that this study was conducted in the fall of 2020, however it was only a few weeks ago that I saw this study in my Twitter timeline and decided to cover it.
The 4 test groups were based on the following:
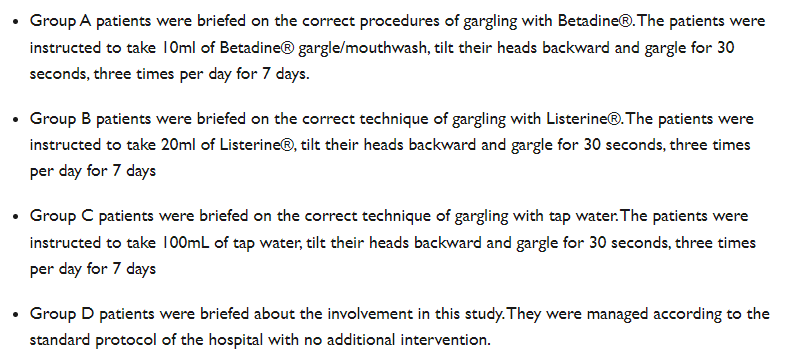
Betadine is the commercial name for Povidone-Iodine, and the use of Listerine was intended to represent the use of an essential oil, more specifically of menthol and eucalyptol which themselves have a long recorded history of being used in herbal remedies due to their antimicrobial activities.
Patients were monitored for viral progression for the first 7 days, although viral clearance was measured through positive PCR tests based on samples taken at day 4, 6, and 12 of the trial.
The results indicate that all of the patients who used Betadine and nearly all of the patients who used Listerine experienced viral clearance by Day 4. What’s interesting is that viral clearance was seen even with some patients assigned to the tap water group.

Care must be taken to reiterate that these studies were done at the very early stage of the disease where patients did not present with any symptoms yet. However, this does lend credence to the idea of early intervention. In fact, in the case of Listerine, it would even point to mouthwash as a possible early treatment that a large majority of people are likely to already have. Like I stated above, many people are likely to already use mouthwash as part of their daily cleaning routine.
If Omicron does target the upper respiratory tract to a greater degree, then not only would there be no harm in using mouthwash but it’s likely to serve some benefit in commonly used oral care routines. The use of Betadine may be more of a concern with respect to possible hyperthyroidism and unfortunately it does not seem like the researchers measured that variable. In order to avoid such a possibility people should reference manufacturer guidelines or guidelines from healthcare professionals. It’s also interesting that even using tap water appeared to have some effect, although it’s hard to discern the data too much when a difference of 1 patient being negative could represent nearly a 20% difference.
So if plenty of people are already using mouthwash how is it that many people are still becoming infected with COVID in real-life? It could be because the mouthwash was used 3 times a day, or that the researchers made sure to use a mouthwash brand known to be both alcohol-based as well as containing menthol and eucalyptol, which have been shown to exhibit in vitro antiviral activities. Again, this is a pilot study that used a very small sample size at the very early stages of the disease so caution should be used when examining the results.
The prior study focused solely on oral rinses. Here’s a recent study where researchers looked at both nasal and oral sprays for their in vitro viricidal properties.
In this study by Meister et. al. researchers took 7 of the most common viricidals on the market, mixed them with SARS-COV2 and a nasal-imitation fluid, and then incubated the solution with Vero E6 cells. Inactivation of the virus was then measured 3 days later. The type of spray and results are indicated below.

From the results of this assay alone, it would appear that only 2 of the products inactivated the virus and reduced the active viral load; Product D and Product I. What’s important here is the distinction between sodium chlorite and sodium hypochlorite, which is more commonly known as bleach. The difference here could likely be attributed to sodium hypochlorite being a stronger base and thus elicits greater viricidal activity. In fact, the use of high salt nasal sprays as viricidal agents are attributed to the conversion of sodium chloride into bleach in host cells more so than the actual inhibitory effects of a high salt environment.
It’s interesting that the researchers did not indicate what type of oral spray they used, but rather hinted that these oral sprays contained essential oils. I couldn’t find a product that would match that combination of both oral spray and essential oil, so I wonder if the researchers may have used those breath sprays that were so popular in the 90s as an oral spray representative.
In regards to the nasal spray results (the products labeled with a superscript C in the chart above), it should be noted that several of these products contain carrageenan and cellulose. The addition of these compounds are not done because they elicit antiviral properties themselves, but mostly because these products create a film along the lining of the nasal passage that inhibits viral particles from crossing into nasal epithelial, essentially acting as a prophylactic barrier. In vitro assays may not be able to capture this nuance well and may not actually be representative of a manufacturer’s intended use of the product.
The researchers made the same remarks in their conclusion:
The application of oral rinses, and nasal or oral sprays could potentially reduce infectious viral loads in the oral cavity, thus temporarily reducing the risk of transmission. Depending on the formulation, oral rinses can impede SARS-CoV-2 infectivity in vitro [5]. In contrast to oral rinses, nasal sprays are not intended to reduce microbial contamination, but rather to promote the detumescence of the nasal mucosa. Moreover, selected nasal sprays contain different types of active ingredients compared with oral rinses, and thus need careful evaluation regarding their inactivation capacity towards SARS-CoV-2. As such, this study investigated seven nasal sprays and two oral sprays regarding their virucidal activity against SARS-CoV-2 during quantitative suspension tests. Nasal sprays based on sodium chlorite, xylometazolin hydrochloride or homeopathic remedies did not reduce virus infectivity, while a nasal spray based on sodium hypochlorite reduced viral loads by 2.21 log10 TCID50/mL (Figure 1B, Product D). In accordance, household and hand disinfectants based on sodium hypochlorite are reported to successfully inactivate a broad range of enveloped viruses [7]. The lithium-magnesium-sodium-silicate within Product D forms a gel matrix that potentially interferes with virus infection due to the formation of an aqueous film. However, further research is required to assess if sodium hypochlorite is well tolerated by individuals in clinical situations. In agreement with previous observations for oral rinses [5], an oral spray containing essential oils completely suppressed SARS-CoV-2 infectivity (Figure 1C, Product I). In the present study, a product containing carrageenan (Figure 1B, Product A) did not harbour any virucidal activity, although recent findings have reported otherwise [8,9]. This discrepancy can potentially be explained by longer incubation times, and a different experimental set-up aiming to evaluate the effect of carrageenan on the viral life cycle rather than a quantitative suspension test.
Overall, this arena of nasal and oral at-home remedies still remains relatively untouched, likely due to the narrative that many of these products are either ineffective or likely to be abused and cause harm to its users. As we have stated, many of these compounds are relatively safe when used as intended by the manufacturer or under discretion by a healthcare worker.
Regardless, at a time where we still have no available, “approved” remedies there should be no surprise that people may turn towards whatever avenues are likely to even have marginal benefits. Even if these at-home remedies may not prove beneficial, many are relatively low risk.
One of the reasons I decided to create this post was due to a Rising video from Kim Iversen, in which she laments the fact that nearly everyone around her was coming down with COVID (both vaccinated and unvaccinated), and yet there were no guidelines or policies coming from the CDC or NIH about how to deal with COVID when ill aside from possibly taking Tylenol. No guidelines on at-home remedies, off-label drugs, or even vitamins! As Kim puts it, people who may feel desperate would rather try something that may have limited benefits rather than nothing at all!
I suggest people watch Kim’s take and understand why, at a point where nearly everyone and their dog is getting COVID that many are frustrated with the lack of any guidance or information in regards to dealing with COVID.
Part III will briefly look at off-label drugs and provide my final remarks on why I decided to make these posts.


The thing that has irritated me the most is the lack of discussion of treatments! Thank you for this.