Clearing the Air
Providing some context to a few circulating misconceptions, including those on "seasonality" and remarks about targeting other SARS-COV2 antigens.
More and more I’m seeing a lot of different ideas and terms thrown out about COVID. Usually, this isn’t a big issue- people should always be allowed to express their opinions, and we generally shouldn’t criticize people for their opinions, period.
However, I’ve growing more concerned that people have generally been inundated with a ton of information but not being able to properly piece the information together.
This seems to be leading people down rabbit holes and ossifying opinions as facts, even when they are not substantiated.
So I wanted to provide some clarity and understanding based on a few things I am seeing. This isn’t intended to target anyone in particular, but are some things I’ve seen in a few comment sections that I think may need a bit of addressing.
The Lack of Seasonality of COVID
With the arrival of COVID there was an idea that we may reach seasonality after a certain amount of time. However, there have been many comments questioning why COVID has not reached seasonality, with many people eventually suggesting that this is caused by the vaccines. There’s a lot to go over here, starting with defining what seasonality is and what other factors may be causing the lack of seasonality.
Seasonality refers to the circulation of viruses during certain months out of the year, rather than year-round circulation. For example, there are certain viruses such as influenza viruses and human coronaviruses that we come across predominately during the colder/winter months.

Seasonality of viruses doesn’t mean that we can’t catch the cold or flu in the summer- it mostly means that infections with these viruses occur predominately at specific times in the year.
There are a few factors that are involved with seasonality, including climate, individual and social behaviors, as well as defenses against the virus (Moriyama, et. al.1):
Accumulating studies point to possible seasonal determinants in the epidemics of respiratory viruses as well as host factors affected by these contributing factors. These include seasonal changes in temperature, absolute humidity (AH), sunlight, vitamin status, and host behavior (8–16). These proposed factors can be classified as seasonal changes of environment, human behavioral patterns, and viral factors (Figure 1). Environmental factors affect host susceptibility by modulating airway defense mechanisms and affect viability and transmission of respiratory viruses. Human behavioral patterns affect the contact rates between infected individuals and susceptible individuals. Among potential drivers of seasonality, fluctuation of temperature and AH throughout the year has been proposed as a critical factor in the seasonal increase in respiratory virus infections, especially in the context of the epidemics in the winter season (12, 15–18).
Or, put in a more condensed manner (Neumann, G. & Kawaoka, Y.2):
(i) virus stability and transmissibility under changing environmental conditions (most prominently, humidity and temperature); (ii) human behavior (including indoor/outdoor activities, indoor crowding, number of close contacts, holiday, and vacation travel, etc.); and (iii) the impact of changing environmental conditions on host defense mechanisms.
The host defense mechanism is the most important part of this discussion.
Virus must overcome many of our own bodies immunological defenses including mucosal immunity, innate immunity, and eventually adaptive immunity. These immunological barriers create filters (also called selective pressures) through which viruses must sift through in order to infect someone.
When a given population is naïve to a specific virus- such as SARS-COV2- then the virus doesn’t have many immunological barriers to overcome. The virus spreads among the naïve population until adaptive immunity increases among the given population.
This is generally what we refer to as herd immunity, although there are many issues with this term3. We won’t be using herd immunity to refer to sterility, but more as a broad term to refer to additional barriers created by adaptive immunity that may lead to bottlenecking and reduced circulation of a virus.
In general, as a population gains more immunity against a virus we create more challenges for the virus to overcome in order to infect us and spread within the population. Eventually, as infection rates decline due to immunological barriers, then the spread of a virus may depend predominately on the other two factors above (climate and human behaviors) and at that point we may consider a virus to be endemic and seasonal in nature. At that point, a virus may become dependent on a few factors such as humidity, temperature, behaviors, as well as slow escape mutations that accrue through antigenic drift in order to gain an advantage over their hosts.
That’s why many flu infections occur in the winter, where low humidity outdoors and high humidity/warmth indoors may create environments conducive to viral spread, including the fact that winter months may lead more people to remain indoors and in closer proximity to others for longer periods may serve as a contributing factor as well4.
Generally speaking, immunological barriers must create a bottleneck before we become concerned about other variables (i.e. the seasonal nature of a virus).
So that brings us to our current predicament with COVID. In essence, why hasn’t COVID become endemic and seasonal?
There are a few reasons, but mostly I would argue that we haven’t reached endemic levels due to having improper immunological barriers due to the sudden gap from Delta to Omicron, as well as all of the Omicron sub-lineages.
Omicron was far too different of a variant. It didn’t follow the typical route of antigenic drift, and instead was a sudden jump more akin to antigenic shift5. What this mean was that prior immunity did not protect against Omicron- nearly everyone, including those who were vaccinated or infected- had a chance of becoming sick.
This was the general problem. Omicron essentially created an immunological redo for the entire world. Most people had to start over since much of the prior immunity did not carry over to an adequate extent. Add onto the fact that lockdowns likely caused many people to become unnecessarily naïve to the virus, and we end up in a predicament in which we need to set up new barriers for the virus.
In order to reach seasonality we need to become immunologically competent against the proper variant, and Omicron has essentially ruined those plans.
So unless we gain immunity against the Omicron variants that confer adequate adaptive immunity, then we may not experience seasonality for some time6.
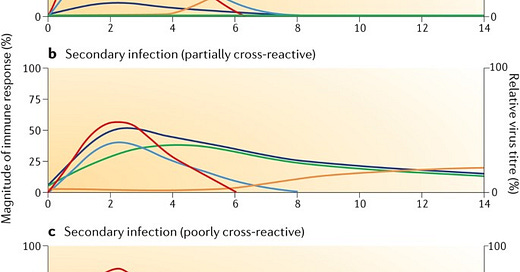
For a conceptual image, I came across this graph which I think shows this scenario really well7.

Usually with antigenic drift a virus may accumulate a few mutations. Although this will always lead to loss of neutralizing antibodies, the cross-reactive antibodies that remain may be enough to confer enough protection (b). However, if the new antigen is too different from prior antigens, then cross-reactive immunity may be greatly dampened, and instead another adaptive immune response must be mounted against the new antigen (c). Essentially, Omicron took us from having population-wide (b) to (c), causing us to have to essentially start over again (relatively speaking).
And if anyone was curious, I generally do not think that the vaccines are what’s stopping seasonality. There are far too many variables we need to work out in order to make such a conclusion. The better argument (for now, I believe) is that Omicron was so different that it created the upheaval and an essential redo immunological-wise.
But this is my perspective on the matter. Let me know if you have other ideas as well.
Targeting another Antigen
This is probably one of the most bewildering comments I’ve seen. Several people, including a few Ph.D’s and M.D.’s have asked why vaccine formulations didn’t target other antigens due to the spike protein’s cytotoxicity.
The main issue with this argument is that the spike protein is THE antigen to target. Full stop. This is legitimately a non-negotiable fact, and the reasons for it rely both on the behavior of the virus as well as the presentation of antigens.
In order to stop a virus from getting into our cells you must target them at their attachment points, which bind to our cells’ receptors. If you target the antigen responsible for attachment, then you stop the virus from being able to bind to our cells. This is generally what is referred to when we talk about neutralization- antibodies target attachment points of a virus and prevent them from infecting cells.
For Influenza A and B the virus is studded with haemagglutinin (HA) and neuraminidase (NA) glycoproteins. The HA glycoproteins are responsible for the virus’ attachment to our cells and entry while the NA glycoprotein is involved with penetration of mucus and cells.

Most neutralizing antibodies against Influenza A and B target the HA glycoprotein. In vaccine formulations for the flu, generally someone is administered either the full virus8 or the HA glycoproteins- not other antigens.
Again, by targeting the HA glycoprotein you can prevent the virus from attaching to cells and thus the infection is halted.
The same goes for SARS-COV2, only for SARS-COV2 the main attachment antigen is the spike protein.
For example, we can take a look at a schematic diagram of a SARS-COV2 virion below9:

And once again, all of the vaccine formulations against SARS-COV2 available either provide the full virus or the spike protein- not other antigens.
In both the flu and COVID vaccines the intent is to halt the virus from attaching, which is why the HA protein of the flu and the S protein of SARS-COV2 are targets.
But there have been a few comments about why we don’t target antigens such as the Nucleocapsid protein of SARS-COV2, especially if such a target may be less cytotoxic.
Well, if we refer to the schematic diagram of the SARS-COV2 virion above you’ll notice the big problem with that question- the Nucleocapsid is sequestered within the virion10.
This presents with 2 main problems.
The immune system needs to see (metaphorically) the antigen that it needs to target. That’s why antibodies generally target surface antigens, and mostly the main antigen responsible for binding to cells. Because the Nucleocapsid protein is located within the virion, there’s no way for the immune system to know that the N protein is there.
Essentially, it can’t target what it can’t see.
But we do produce antibodies against the N protein after a natural infection, so the N protein does have to make itself known at some point.
This is part of the second problem- the N protein doesn’t become known to our immune system until the viral infection is well underway.
At the point that our body recognizes the N protein, we’re likely to have been infected for quite some time. Protein production of viral antigens during replication will lead to the production of N proteins, and if a host cell lyses then the N protein may spread into the extracellular environment. At that point the immune system may recognize the N proteins and mount an adaptive immune response against said N proteins.
Those antibodies will then target the N proteins, but is that targeting necessary? Again, if the N protein exhibits its own cytotoxicity then hindering the protein may reduce cellular damage, but with respect to stopping an infection or halting the virus targeting the N protein won’t do any good. The virus would have been replicating for some time, and targeting the N protein won’t stop future viral entry and replication.
That’s why we don’t target other antigens including the N protein- they won’t stop the virus from replicating.
I’m not sure why this isn’t known to many, yet I continue to see comments brought up as to why we don’t target other proteins such as the N protein. It’s for the reasons above that we focus almost all of our attention towards the spike protein. Unfortunately, the spike protein undergoes a high degree of mutations, meaning that any protection we get may not last very long. It also confers some of the most cytotoxic effects on our cells.
It’s why I’ve used the paradoxical phrase that the cure is the disease. The antigen that we need to target is the one that is likely to be causing harm to our bodies, and so any exposure to the spike may be harmful.
But that doesn’t mean we can just look at other antigens to target. It doesn’t work that way because our immune systems don’t work that way. It can’t figure out that the N protein is located inside of the SARS-COV2 virion, and antibodies most certainly can’t dig their way into the virus to reach the N protein. And even if antibodies could, the virus will still be able to bind because the S protein would not be hindered.
This is a general problem where we must remember what the antigen does and where it resides on or within the virion. In figuring this out, we can understand why we are in the predicament that we are in, and why it would be nonsensical to target other antigens such as the Nucleocapsid protein.
Apply the Knowledge
There are a few more examples that I may get to at some point. More and more it appears that many people are gathering more information, which itself is absolutely great.
However, for some it doesn’t appear that they are applying the information in a proper manner. It’s not enough to have the information, but to know how to use that information to tie ideas and concepts together.
Be careful in becoming a passive reader that just looks at the information and provides minor quips. We’re not sponges, and so don’t just absorb the information. Use that information, look around and see what may be going on. Instead of deferring to snarky comments, spend some time and see if you can piece together what you see in a useful manner. Ask pertinent questions. In fact, always ask questions, especially if the information you are presented with may not make sense.
Learn, grow, and apply- do not become static. We are reaching more than 2 years post the start of the pandemic. That means we should have two years of knowledge, with two years of information to tie together.
But with that said, I’d like to hear from you all. Are there a few things you are noticing that you would like some clarity on, or anything you may have questions about. Please let me know in the comment section below!
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

Moriyama, M., Hugentobler, W. J., & Iwasaki, A. (2020). Seasonality of Respiratory Viral Infections. Annual review of virology, 7(1), 83–101. https://doi.org/10.1146/annurev-virology-012420-022445
Neumann, G., & Kawaoka, Y. (2022). Seasonality of influenza and other respiratory viruses. EMBO molecular medicine, 14(4), e15352. https://doi.org/10.15252/emmm.202115352
There’s a general issue with how herd immunity is used in lay speak. It doesn’t refer to immunity that confers sterility against a virus, nor is there any specific percentage to which we can attribute to the population. Did you ever wonder where the supposed 70% herd immunity comes from? Scientists generally aren’t getting these numbers by letting out a herd of animals (or humans), providing them either vaccination or natural immunity, and then measuring to see if the virus has been attenuated within this population. The percentage generally comes from mathematical modeling, and so this is a general issue in which math models (which serve to be a predictive framework) are adopted and eventually co-opted to mean things vastly different from the initial meaning. I came across this issue when describing leaky vaccines, which themselves are defined in lay terms but derive their definition from mathematical modeling.
Brian Mowrey wrote up an interesting piece on herd immunity in the current climate.
Much of the discussion on seasonality can get very technical. The Moriyama, et. al. paper has a good in-depth analysis of all of the factors including heat, pH, humidity, and droplet size and how this affects transmissibility of a virus.
The concepts of “drift” and “shift” are usually used to define flu virus antigens. Drift usually refers to small mutations that lead to small changes in the flu virus’ surface antigens. Generally the move from Wuhan → Alpha → Beta would be considered some form of antigenic drift.
Shift, on the other hand, defines a sudden or massive change in the surface antigen. With the flu virus this usually occurs due to recombination between different flu variants or through a jump from one species to another. The jump from Delta → Omicron for COVID can’t be defined by antigenic drift even if we assume natural origins of Omicron. If from an animal reservoir, that argument would still itself point to some form of antigenic shift rather than drift. In general, shift would at least suggest that the differences between Delta and Omicron are so drastic that we can’t make comparisons to pre-Omicron variants.
For anyone who may be confused, here’s a comment I gave to Clarisse in a prior post for those looking for something succinct:
Well I think the biggest issue is that we don't know which direction Delta would have gone because of the abrupt emergence of Omicron. This is one of the reasons why I'm critical of such comments such as the lack of seasonality for COVID. Well, seasonality requires that the virus circulate among the population until competition between the two causes it to plateau in some way. Omicron didn't allow us to reach post-Delta variants that may lead to seasonality, and now we're dealing with sudden jumps between Omicrons which are likely to have been around at similar times to one another.
Petrova, V., Russell, C. The evolution of seasonal influenza viruses. Nat Rev Microbiol 16, 47–60 (2018). https://doi.org/10.1038/nrmicro.2017.118
Note that the presentation of the whole virus within a vaccine is not intended to elicit antibodies against all of the virus’ antigens. The intent is to still mount a response against either the HA glycoprotein of Influenza A and B or to mount a response against SARS-COV2’s spike protein. The idea here is still consistent with antigen-only vaccines.
Lee, Cheryl & Lin, Raymond & Renia, Laurent & Ng, Lisa. (2020). Serological Approaches for COVID-19: Epidemiologic Perspective on Surveillance and Control. Frontiers in Immunology. 11. 10.3389/fimmu.2020.00879.
Although the Nucleocapsid protein has been found to have some cytotoxic effects in vitro, the main purpose of the N protein is to help coil up the viral RNA in a manner similar to our own histone proteins that wind up our DNA. The N protein helps to make the viral RNA more compact and fit inside the virion.




Great article, 10 out of 10. You and Brian are on a tear.
100% agree on the N protein. The N protein antibody is an indication of a broad immune response -- not really a great weapon in the fight against the virus.
If the S protein antibody is a rifle that can engage the enemy and keep him away -- the N antibody is at best a bayonet that you can use if the enemy is inside your quarters and you are running out of bullets.
What I understood through the pandemic is that the science is only beginning to lift the veil on how our immune system works and scientists use tidbits of knowledge to poke around in the dark. (This is why Warp Speed was a terrible idea and a cover the the already pre-made vaccine) This is okay since science takes time to develop, we just need to be aware of it.
But I broadly do not understand what our immunity to Sars-Cov-2 even IS.
Why, say, among the below constantly exposed people there is a diference:
- unvaccinated Adam had no covid ever
- unvaccinated Igor had only one Covid in Nov 2020 despite being out and about
- unvaccinated Bob had three Covids
- Vaccinated Charles had vaccine and no covid
- Vaccinated David had vaccines and multiple covids
What is it that is different between those persons? I am not entirely stupid and ignorant and I can observe differences betwen classes of people and how vaxed people seem to get reinfected more often. But while I have some observations and ideas that I posted on my substack, I also realize that I have much to learn.
For example: can someone get reinfected with the SAME variant as their last Covid, if we tried to infect them on purpose, say half a year after last infection, using a lab solution of their own specific virus that this person had 6 months ago.
Etc
Many questions that I do not see answered. Wondering what you think
Why not target the membrane or envelope proteins then?
Why aren't they getting a mention?
Are they more stable to mutating?
Even if they were prone to mutating it would give more options for the immune system surely... thus less likely for the whole virus to escape it...(?)