Yes, Obesity can Affect Vaccine Effectiveness
It should be no surprise that an altered immune state should affect vaccine-induced immune responses.
In a previous Substack piece I lamented the fact that we seemed to have become a culture focused on hedonism and consumption. Even during a pandemic we seem to have paid very little attention to our own weight and to the weight of those around us and in the nation at large.
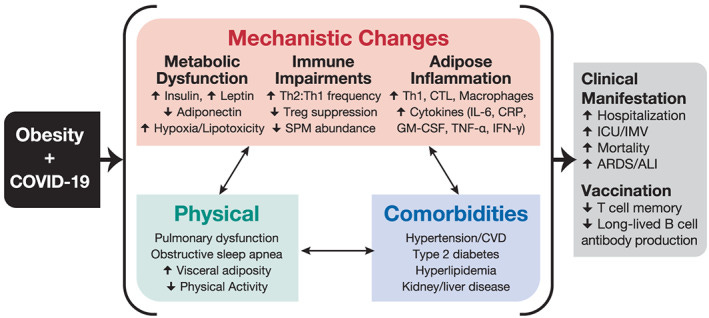
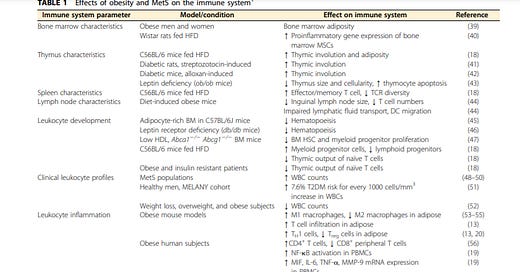
There’s plenty of evidence that indicates that obesity can have severe consequences when it comes to a functioning immune system, and is a large contributor to other maladies.


It makes perfect sense to then argue that impaired immune function will lead to greater severity of illness. This case was made very apparent during the 2009 H1N1 epidemic, where the number of obese hospitalized/deceased patients was so high that obesity was counted as its own independent variable.
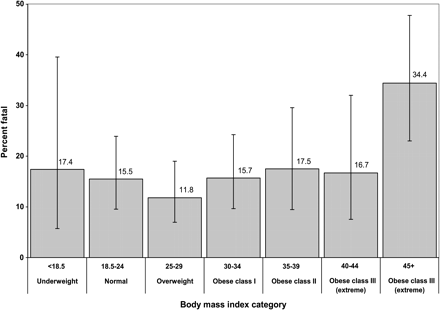
A study conducted by Loui et. al. 2011 indicated the strong prevalence of H1N1 infection in obese populations (emphasis mine):
The prevalence of BMI ≥40 (19%) was at least 2.5 times higher than the estimated prevalence in the United States (2.8% of US men and 6.9% of US women), and the prevalence of BMI ≥45 was at least 10-fold higher than national estimates (11.3% vs 1.1%) []. Obese persons were also more likely to die once hospitalized due to 2009 H1N1 infection. After adjusting for co-morbidities and other risk factors, extreme obesity (BMI ≥40) was independently significantly associated with death due to 2009 H1N1 infection. In addition, further sub-analysis demonstrated that case patients with BMI ≥45 had a 4.2-fold increased odds of dying, with a case-fatality proportion of 34%. A model using an upper threshold of BMI ≥50 showed similar odds of death as a model using an upper threshold of BMI ≥45 (data not shown).
There’s a large body of evidence suggesting that obesity can have severely negative outcomes when it comes to disease due to compromised immune function, but what’s even more concerning is that a compromised immune system will also mean that vaccines will not be as effective. This is a huge concern when a large portion of the American population are either overweight or obese, and continue to gain more weight over the course of the pandemic.
In a study conducted by Sheridan et. al. 2012, scientists looked to see if obesity would lead to decreased protection from influenza vaccines by measuring antibody titers after 12 months and by measuring CD8+ T-cell expression (emphasis mine):
Our data show that obese individuals mount a vigorous initial antibody response to TIV. However, a vaccine is protective only if the antibody titer is maintained throughout the period when influenza virus is circulating in the population. To examine the level of antibody maintenance after vaccination, we measured antibody levels 12 months after vaccination. Increases in BMI were positively correlated to decreases in antibody titer. More than 50% of the obese participants had a ⩾4-fold decrease in HAI titers to A/Brisbane/10 and B/Brisbane/60, and 47% had a ⩾4-fold decrease in HAI titer to A/Brisbane/59 at 12 months compared with 1 month post vaccination. By comparison, <25% of healthy weight participants had a >4-fold decrease in HAI titer to A/Brisbane/59 and B/Brisbane/60…
We found that percentage of influenza-activated CD8+ T cells were decreased in the obese participants, and two markers of functional CD8+ activity, IFNγ and granzyme B, were also significantly decreased in the obese participants. CD8+ T cells kill virus-infected cells by release of perforin and granzyme B26 and inhibit viral replication by the release of IFNγ.27 The fact that influenza-stimulated CD8+ T cells from obese individuals were deficient in the expression of both of these proteins strongly suggests that protection from an influenza infection may be not be optimal in the obese population.


The ramifications here are enormous, and what’s more alarming is that they have been well-known. We have known for many years with a ton of evidence that obesity leads to severe prognosis and worse illness outcomes.
We know that this stems from a compromised immune system that is unable to function properly to clear out infections or mount a robust response against pathogens. What seems to not be known is the connection between a compromised immune system and vaccination, but the evidence has always been there and the inferences can be easily drawn; vaccines are intended to stimulate an immune response to create antibodies and proper T-cell expression.
It should seem obvious then that a compromised immune system that has difficulties eliminated pathogens will also have difficulties mounting a proper immune response towards vaccinations.
As indicated in Kwok et. al. 2020 (emphasis mine):
Lower vaccine efficacy has been reported in people with obesity following the H1N1 pandemic. 38 While there was no significant difference in antibody titres between people with obesity and healthy‐weight individuals 1 month after H1N1 vaccination, people with obesity had a 4‐fold or greater decline in antibody titres compared to healthy‐weight individuals at 12 months post‐vaccination. 129 Obesity is associated with T cell dysfunction and the impaired response means a proportion of individuals with obesity remains at risk of influenza despite vaccination. 130 A similar risk with a future COVID‐19 vaccine would be concerning. Importantly, the typical participant in the recently published early phase trials of vaccines against SARS‐CoV‐2 was normal weight. 131 , 132 , 133 Although these trials have shown promising results, applying their findings to populations with high background prevalence of obesity – 40% in the United States, 29% in England and 13% globally – carries a degree of uncertainty which may hopefully be addressed in Phase 3 trials.
And also iterated in Milner et. al. 2012 (emphasis mine):
Vaccination is universally recommended by public health officials to combat several types of infections. However, there is some evidence suggesting that obese individuals may not respond to vaccination to the same extent as healthy-weight individuals. Obesity was associated with a poor antibody response to hepatitis B vaccination(42,43). Additionally, overweight children displayed considerably lower anti-tetanus IgG antibodies in response to vaccination compared with healthy-weight children(44). This reduced immunogenicity in response to vaccination could be caused by several factors. One possibility is impaired generation and/or function of the antibody-secreting plasma cells. Another factor could be reduced absorption of the vaccine at the site of injection due to excess adiposity(44). Interestingly, a recent study reported that using a larger vaccine needle length resulted in considerably higher antibody titres to hepatitis B surface antigen in obese adolescents(45). As mentioned, poor response to vaccination has important public health implications. Reduced protection against viral infections, such as hepatitis B, increases individual susceptibility and may increase the likelihood of transmission to others. Therefore, more research on how obesity may negatively impact vaccination response is necessary to ensure proper protection in this at risk population.
Over the course of this pandemic we have all witnessed the lack of a comprehensive, transparent campaign in response to SARS-COV2. The narrative has focused on a one size fits all approach and has not provided any area for nuanced, individual-driven approaches to tackling the disease. There’s no doubt that this issue has been amplified with the rampant mass vaccination campaigns that we have all been subject to.
When the only position we have taken against fighting this disease is to focus solely on mass vaccination, we miss out on all of the other issues that can greatly alleviate hospitalizations and death. Nowhere do I see a similar massive campaign to encourage weight loss, proper eating, exercise and supplementation. Instead, as outlined in my previous Substack, we see the opposite argument occurring where we are being intentionally dissuaded from drawing any parallels between COVID-19 hospitalizations and obesity in an attempt to be sensitive to the body positive crowd.
This lack of transparent data will no doubt have serious ramifications when it comes to vaccinations. I have outlined above that there is robust evidence that vaccines may not be as effective the higher someone’s BMI is. This runs absolutely counter to the narrative of mass vaccination when we do not consider obesity as a variable but expect everyone to get the same dosage and vaccines.
What’s even more alarming is that we are entering into a realm of providing special privileges to those who are vaccinated, such as providing them the ability to not wear masks in stores or providing vaccine passports as a gateway to social activities. If the argument here is that we need to reach herd immunity as quickly as possible, and we naively ignore the notion that a large group of vaccinated, obese people may have a strong chance of becoming infected and thus infect others due to weakened & waning immunity, we may run into an issue where we are leading people to wrongly assume that they are strongly protected against catching COVID. Now that we are seeing strong evidence of waning immunity among many vaccinated individuals, we need to be even more transparent about the factors that alter a vaccine’s effectiveness.
I have seen this approach be taken by many people; I am obese, am at increased risk for becoming seriously ill with COVID, therefore I should get vaccinated. I am not arguing against one’s personal decision to get vaccinated, and the idea here would seem valid, but the approach is heavily misguided.
Not only should we make sure that people understand their risks of getting ill if they catch COVID, but that they may not be fully protected by vaccinations due to their weight. An informative, robust campaign that alerts people to this concern, to alert them that their best way of tackling COVID should also include maintaining a proper weight and a large emphasis on self-improvement, will be the best way of fighting the disease. With respect to vaccinations in general, we may have to take into consideration different variables such as dosages, method of inoculation, and timing of vaccination when we account for different groups such as the obese.
When presented with information we seem to have lost the ability to draw parallels and connect the proper dots. The relationship between disease, vaccines, and obesity should seem very obvious to anyone who is willing to look at the information. In a culture that argues against independent sensemaking we may find ourselves in a position where we are unable to properly comprehend the information that is presented to us, and we may cloud out many variables that we should be engaging with.
More logical thought should always be welcomed, and we need more of it now than ever before.
Thank you for reading my newsletter. If you enjoy my articles please consider becoming a free subscriber in order to receive notifications.
And share with others who may find these newsletters interesting.
Also, please consider becoming a paid member. The research and work put into these articles takes many hours and being a paid subscriber allows me to continue to do this full time.
In-Text Citations:
Andersen et. al. 2016. Impact of Obesity and Metabolic Syndrome on Immunity1,2. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4717890/
Kwok et. al. 2020. Obesity: A critical risk factor in the COVID‐19 pandemic. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7460880/
Popkin et. al. 2020. Individuals with obesity and COVID‐19: A global perspective on the epidemiology and biological relationships. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7461480/
Louie et. al. 2011. A Novel Risk Factor for a Novel Virus: Obesity and 2009 Pandemic Influenza A (H1N1). Taken from https://academic.oup.com/cid/article/52/3/301/307314
Sheridan et. al. 2012. Obesity is associated with impaired immune response to influenza vaccination in humans. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3270113/
Milner et. al. 2012. Micronutrients, immunology and inflammation The impact of obesity on the immune response to infection. Taken from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4791086/




Recently I came across how antibiotic use and exposure during early childhood development (up to age 3) can alter the gut microbiota (dysbiosis) and establish a predisposition to obesity in children and adults. Studies in the last decade have pointed to this disruption in our flora due to antibiotics, which contribute to promoting certain bacteria that "affects energy harvest from the diet and energy storage in the host". It's really quite the eye opening area of research and shows the interconnection between seemingly separate health problems. Antibiotic misuse and overuse, poor dietary nutrition (including high-fructose sweeteners, excessive simple carb consumption), Vitamin D deficiency from ongoing dietary imbalances and lack of basic sunshine, increasingly inactive lifestyle in ratio to caloric requirements. All these issues are interacting and compounding the problem of so-called Covid-19 immunity... yet the one size fits all vaccine answer is our only hope? Yikes!