The IgG4 situation is highly complex
Let's avoid simplistic associations when examining the information for answers.
IgG4, IgG4, IgG4! It’s all about IgG4!
The revelations of a months-old pre-print, but just formally published article in Science has caught many people by storm with respect to IgG4.
The findings are unprecedented, because IgG4 is considered an odd antibody which not much is fully known.
And because of its oddities, along with concerns over the vaccines, many people have gone down wild goose chases examining this antibody, looking at various diseases that are associated with IgG4 such as cancer and systemic fibrosis and suggesting that IgG4 production from the vaccines will spell cancer and other maladies for millions worldwide.
A problem with this thinking is one that has generally plagued COVID discourse, in that it takes highly complex ideas, of which much is unknown, and attempts to boil it down in order to provide people with answers.
This process of showing people what to think, rather than how to think means that many people will sop up information and use it as they are being told to, without so much as thinking of the underlying mechanisms or how to piece information together into a broader concept.
Even with this novel finding it’s important to remember that these events are highly complex, and we lose out on a lot of the nuances when we start throwing everything at the wall in order to see what sticks.
Which came first; the antigen or the antibody?
What I find so strange is that many people have scoured around for papers on IgG4 such as cancer and have used this as an indication that the vaccines will cause cancer.
Are the vaccines the reason cancer is on the rise? Quite possible, but the issue here isn’t about this hypothesis alone, but the ties made to make such inferences.
The general consensus around IgG4 class shifting is that persistent presentation of some antigen is what causes the class shifting, as if the persistent pestering of the immune system to deal with an issue shuts off effector function since it’s not worth the hassle.
In the case of cancer, the formation of IgG4 antibodies is a consequence of the tumor. As tumor cells grow and replicate, the immune system attempts to kill off the cells using cell-mediated cytotoxic processes.
However, if the tumor cells multiply far more quickly than the immune system can fight them off, then class shifting towards IgG4 may occur, as noted in a diagram from Crescioli, et al.1
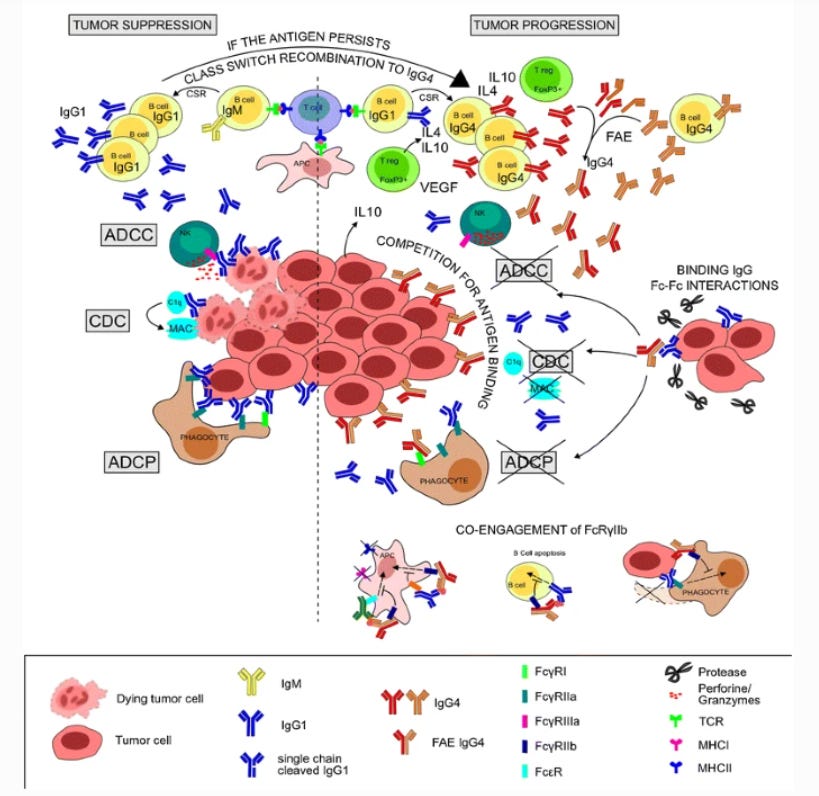
Unfortunately, this class shifting as it relates to cancer can aid in tumor progression, rather than attenuate it.
If we look at this new term IgG4-Related Diseases (IgG4-RD), note that the disease is of unknown etiology. That is, most researchers are unsure what is causing the IgG4 production, but it’s suggested that it has to come from some antigen, possibly an autoantigen that the body has targeted over a long period of time and through chronic inflammation.
One cited review from Della-Torre, et al. (2015)2 notes several times throughout that the antigen for IgG4-RD tends to be unknown:
Little is known with certainty about the pathogenic events that initiate IgG4-RD. The evidence of common histopathological features shared by different unrelated organs suggests that IgG4-RD might be an antigen-driven inflammatory condition leading ultimately to tissue fibrosis. However, a number of unsolved questions still need to be addressed, including: (i) the pathophysiological importance of IgG4 antibodies; (ii) the characterization of the putative microbial or self-antigen; (iii) the imbalance between T helper type 1 (Th1), Th2 and regulatory T cell activation; (iv) the role of innate immunity; and (v) the immunological mechanisms leading to fibrosis.
This sentiment is found in many IgG4-RD articles, in that most researchers aren’t exactly sure what antigen these individuals are constantly being exposed to.
But in any given case, the important fact here is that IgG4 class shifting is downstream of repeat exposure to an antigen. It’s the fact that some individuals are exposed to an antigen that causes the class shifting towards IgG4.
This is important to highlight, because when we look at studies it’s easy to look at the presence of IgG4 and immediately infer that the IgG4 is the cause of the maladies.
In reality it may be a witness to the crime scene, where detectives show up and immediately point fingers at the antibody drinking a Big Gulp on the corner, because of course the suspect always returns to the scene of the crime!
It’s strange if the suspect happens to be around at every crime scene, but it’s also incorrect to suddenly implicate someone as a suspect just because they were around.
This is one of the issues when many people have cited a correlation between IgG4 levels and mortality in SARS-COV2 infected people.
Similar researchers from the Footnote #2 study provided a SARS-COV2 prospective analysis3 in which they found higher rates of mortality in IgG4 elevated individuals compared to those with less elevation, suggesting a correlation between IgG4 levels and prognosis:
In this prospective study we found that serum IgG4 level predicts a poor COVID-19 outcome. Based on the available literature, IgG4 antibodies may contribute to COVID-19 progression via at least two possible mechanisms, yet to be verified. Because anti-spike IgG4 have shown poor in vitro neutralizing capacity compared to IgG1, IgG2, and IgG3 antibodies, a first possibility is that hosts with prominent IgG4 immune responses might be more permissive to SARS-CoV-2 infection [6]. On the other hand, as neutralizing anti-IFNγ autoantibodies observed in adult patients with multiple opportunistic infections are predominantly of IgG4 subclass, it is tempting to speculate that anti-IFN antibodies associated with impaired anti-SARS-CoV-2 immunity and life-threatening COVID-19 pneumonia might also be IgG4 [7]. Despite intrinsic limitations mainly related to the limited number of patients enrolled, our study identifies IgG4 antibodies as a possible additional overlooked variable of the humoral immune response against SARS-CoV-2 associated with COVID-19 progression.
The researchers don’t provide any information on time between infection and arrival at the hospital, and there’s no explanation for the strict cutoff of 700 mg/L of IgG4 to categorize a patient as being elevated or not elevated.
What’s interesting is that treatment for IgG4 and IgG4-RD tend to utilize glucocorticoids as a go-to method with fairly good results, and in this analysis the researchers note that patients were given dexamethasone upon arrival. In fact, many hospitals prescribes dexamethasone and other glucocorticoids at admission, although dosage has been heavily criticized for being too low to have any clinical effectiveness (6 mg/day given intravenously for 10 days in this study).
All this to say that the researchers here are also implicating IgG4 as the being attributed to COVID severity, when in reality it’s also plausible that the presence of elevated IgG4 may be indicative of immune dysfunction, such that some people’s immune systems immediately move towards class shifting rather than effector function and cell-mediated targeting of the virus.
Again, the presence of IgG4 may be downstream of immune dysregulation, and it may be the immune dysfunction that may tell us why some people do worse than others with COVID, rather than the activities of the IgG4 themselves.
This is another example of how correlation not being causation may lead to misdirections in interpreting data.
As it relates to cancer and IgG4-RD, it’s possible that systemic circulation of IgG4 is secondary to a localized, focused response to cancer or an autoimmune disorder before the widespread IgG4 is found.
In that respect, it’d be interesting to see if IgG4 is a contributor to cancer metastasis, in which circulation of IgG4 from a local region, along with cancer cells, may help aid in the cancer seeding ground in other tissues.
And so it’s quite possible that circulating IgG4 occurs only have continuous, local IgG4 class shifting.
But again, much is still not know in regards to IgG4 or IgG4-RD, and so to argue to what degree of pathogenicity IgG4 may cause to the body is still up for debate.
Everybody is different
An issue with many scientific studies is that they tend not to tell us the story of an individual patient.
We tend to get some demographic information, but nothing of the sort that provides personal, longitudinal data about what goes on in individuals.
We got fairly close a few months ago with a study that looked at the immunological profile of individuals who were infected with COVID:
This was a unique study because it provided humoral and innate immune profiles for individuals, and actually allowed you to see how differently people respond to COVID by stratifying the information for each subject.
And we all, in fact, respond differently from one another, including production of IgG4 and class shifting.
We can see this in the supplementary material from the IgG4 study (Figure S3.B) which maps longitudinal changes in memory B-cells as ratios between IgG4 and other IgG subclasses. Note that for some people IgG4-specific memory B cells increased with each vaccination, some decreased with each vaccination, and for some individuals a weird V-shape can be seen:
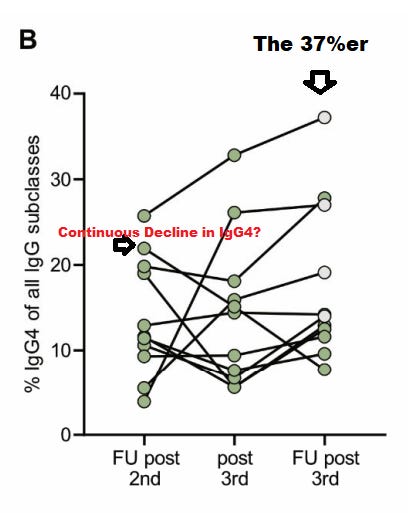
The one individual that appears to have started with a relatively high %IgG4 that declines is really interesting (the person right above the 20% mark), and why such a V-shape appears for individuals is also strange, as if to suggest that days after the booster a maturation of memory B-cells for other IgG subclasses are occurring.
It’s also important to point out that the 37% IgG4 mentioned in the article refers to that one individual who continued to show elevated IgG4 levels (emphasis mine):
While the frequency of IgG4-expressing memory cells among non-spike binding memory B cells was in the range of 1–8% as described before (28), a significantly higher frequency of spike-binding memory B cells expressed IgG4 at all time points, reaching up to 37% of all IgG subclasses (Fig. 2B; Fig. S3). As expected from serological data, IgG3 was underrepresented and considerable frequencies of IgG2-positive memory B cells were found among spike-binding memory B cells (Table S2).
So it’s a bit disingenuous for the researchers to argue that IgG4 levels reached up to 37% when this appears to be the case in one individual and around the teens for others.
But what’s important here is that not everyone produces the same levels of IgG4.
Why is it that some people continue to show high levels of IgG4 while others show a decline, starting with a high number right off the bat but going down with each vaccine?
This is a problem when we look at a study, generalize the findings and make broad-stroke assumptions.
In lieu of some of this information and trying to piece them together, I’m actually curious as to whether the IgG4 class shifting from vaccination may be a predictor of those with immune dysfunction.
That is to say, that those who show high levels of class shifting may also have immunological issues (whether known or not).
This would coincide with the findings from the Della-Torre, et al. (2021) study and the correlation between IgG4 levels and mortality.
Put another way, people who show such high IgG4 levels such as the 37%er above may be more predisposed to severe COVID, and quite possibly other illnesses due to some other factors.
Of course, all of this is speculation and would need to be corroborated with actual evidence. The 37%er above had COVID, yet we don’t know how severe of an infection this person had.
But given that we don’t have individual demographic information, and that the researchers provide very little demographic information overall, it’s hard to tell exactly what underlying factors may contribute to this IgG4 phenomenon.
It’s all a matter of perspective
There’s a lot more to be said about IgG4, including one article4 suggesting that non-specific IgG4 may bind to cancer-specific IgG1 and may inhibit effector function that way (thanks to Jim H in Brian’s comments for pointing out this study).
This nondiscriminatory action of IgG4 would be concerning. However, that would have to take into account what produces IgG4. If many things produce IgG4, then this is a rather broad issue that would implicate all matters of IgG4 production and would possibly make the vaccine-related IgG4 production not as severe (although strange and still worth investigating).
In keeping with the theme of microbiome posts, there appears to be an association between IgG4-RD and commensal bacteria (Hsieh, et al.)5:
Haruta et al. [20] have explored the potential effect of chronic exposure (1 week ~12 months) of a mouse model to killed E. coli in the pathogenesis of IgG4-RD. They have concluded that a persistent stimulation of pathogen-associated molecular pattern (PAMP) activator to innate immune system may ultimately lead to the occurrence of AIP associated with salivary gland lesions which is probably through molecular mimicry. Yanagisawa et al. [21] have further identified the outer membrane protein flagellin (FliC) of the commensal flora could induce AIP-like pancreatitis with generation of high titer of anti-lactoferrin and anti-CA II antibodies in mice after repeated inoculation. These results emphasize the importance of commensal bacteria in inducing AIP via PAMP recognizing receptors. Following this way, many authors have also demonstrated that intestinal commensal microflora-released danger-associated molecular pattern (DAMP) activator can bind to Toll-like receptors (TLRs) or nucleotide-binding oligomerization domain-like receptor (NOD-like receptors, NLRs) on basophils to skew naïve T lymphocytes to Th2 responses for the development of IgG4-RD [22,23,24,25,26].
So maybe our own microbiome can contribute to IgG4 production. Some studies have indicated that the microbiome of those with IgG4-RD are different than others, and so maybe certain strains may contribute to this strange class shifting. Of course, people who have IgG4-RD also suffer from chronic inflammation, and the inflammation itself can alter the gut microbiome, so this is also another issue of figuring out the chicken vs the egg.
In any case, the IgG4 phenomenon is only as concerning as the information that we are presented.
Right now many people have presented associations with cancer or fibrosis, which may appear scary, but without any other additional context people may only be able to look at IgG4 from that scary perspective.
It’s a matter of what information we are presented with that shapes our perspective, and when we are provided only very little information it’s easy to make assumptions that can seem fearful.
Know that this vaccine IgG4 study is the only one of its kind. Without any other information to work with we won’t know the significance of this study. Other studies may corroborate these findings, but others may rebut them. This is a critical time when reproducibility in science is needed so we can see whether other researchers can get similar findings.
Note now that many people are chasing after IgG3, as if to say that IgG3 is the most important antibody in fighting SARS-COV2, with a few people citing this study from Kroger, et al.6 as being the main reason for IgG3's significance.
However, Kroger, et al. themselves even note that their findings run counter to other findings out there, noting the significance of the other IgG subclasses:
In contrast to our study, in which IgG3 was found to be the most important IgG subclass for neutralizing SARS-CoV-2, a number of smaller studies have found that IgG1 plays a more important role [20–22]. Klingler et al. analyzed samples from 29 convalescent donors and found that IgM and IgG1 had significant neutralizing activity against the spike and RBD of SARS-CoV-2; whereas IgG3 had significant neutralizing activity against the spike protein, but not the RBD [23]. Luo et al. analyzed data from 63 convalescent donors who experienced severe, moderate, mild and asymptomatic COVID-19. Luo et al. found that both IgG1 and IgG3 were key to the humoral immune response [24]. In addition, Mazzini et al. analyzed 181 human serum samples using commercial and in-house ELISA assays, and found that IgG1 and IgG3 had the strongest reactivity to the SARSCoV-2 antigens spike S1 and spike-RBD [25].
Rather than figure out why such discrepancies exist, people are now assuming that IgG3 is the most importantest antibody out there because…some people said so? Or maybe because this one study says so?
It’s an issue when studies are looked at with a heavy recency bias, in which we only consider the most recent studies in our assessments, rather than the totality of the studies available.
So remember that all of this is a matter of perspective. Things only appear a certain way if one is only presented with select information.
Always seek out additional information and piece things together.
With that, if anyone has anything else in regards to IgG4 they would like to discuss please comment in the comments section. I may return to IgG4 some time in the future after I finish the things already on my table, but I would like to see other people’s thoughts on this matter, including any additional questions.
If you enjoyed this post and other works please consider supporting me through a paid Substack subscription or through my Ko-fi. Any bit helps, and it encourages independent creators and journalists outside the mainstream.

Crescioli, S., Correa, I., Karagiannis, P. et al. IgG4 Characteristics and Functions in Cancer Immunity. Curr Allergy Asthma Rep 16, 7 (2016). https://doi.org/10.1007/s11882-015-0580-7
Della-Torre, E., Lanzillotta, M., & Doglioni, C. (2015). Immunology of IgG4-related disease. Clinical and experimental immunology, 181(2), 191–206. https://doi.org/10.1111/cei.12641
Della-Torre, E., Lanzillotta, M., Strollo, M., Ramirez, G. A., Dagna, L., Tresoldi, M., & COVID-BioB study group (2021). Serum IgG4 level predicts COVID-19 related mortality. European journal of internal medicine, 93, 107–109. https://doi.org/10.1016/j.ejim.2021.09.012
Wang, H., Xu, Q., Zhao, C., Zhu, Z., Zhu, X., Zhou, J., Zhang, S., Yang, T., Zhang, B., Li, J., Yan, M., Liu, R., Ma, C., Quan, Y., Zhang, Y., Zhang, W., Geng, Y., Chen, C., Chen, S., Liu, D., … Gu, J. (2020). An immune evasion mechanism with IgG4 playing an essential role in cancer and implication for immunotherapy. Journal for immunotherapy of cancer, 8(2), e000661. https://doi.org/10.1136/jitc-2020-000661
Hsieh, S. C., Shen, C. Y., Liao, H. T., Chen, M. H., Wu, C. H., Li, K. J., Lu, C. S., Kuo, Y. M., Tsai, H. C., Tsai, C. Y., & Yu, C. L. (2020). The Cellular and Molecular Bases of Allergy, Inflammation and Tissue Fibrosis in Patients with IgG4-related Disease. International journal of molecular sciences, 21(14), 5082. https://doi.org/10.3390/ijms21145082
Kober, C., Manni, S., Wolff, S., Barnes, T., Mukherjee, S., Vogel, T., Hoenig, L., Vogel, P., Hahn, A., Gerlach, M., Vey, M., Widmer, E., Keiner, B., Schuetz, P., Roth, N., & Kalina, U. (2022). IgG3 and IgM Identified as Key to SARS-CoV-2 Neutralization in Convalescent Plasma Pools. PloS one, 17(1), e0262162. https://doi.org/10.1371/journal.pone.0262162






Great article. I had reasons why I did not mention IgG4-RD (IgG4-related disease) and IgG4 in late stage cancer, in my latest article. Thank you for pointing out that IgG4-RD is unrelated to Covid vaccine findings, and late stage cancer is the horse that pulls the IgG4 cart, not the other way around.
I hope for more research into this topic.
Considering changing my name to IgG4or (just kidding)
The only conclusions anyone should be jumping to is that the jabs are neither safe nor effective. In fact, they have proved to be downright lethal, IgG4 or not.