The Fluvoxamine Anthology Series Archives
A Collection of Fluvoxamine Posts including the "Pseudoinfection" Hypothesis & Citations
This post was copied and pasted over from Modern Discontent. If you are interested in Anthology Series posts as they come in or are interested in smaller posts along the way please consider subscribing over there as that is the main Substack. Also, paid-only content will only be available through becoming a paid member on Modern Discontent.
I hope you’re all not exhausted from all of the posts! Fluvoxamine has fallen into infamous category of repurposed COVID drugs that may never see common use. It’s an SSRI that has been in use for several decades for the treatment of depression as well as other neurocognitive impairments. Overall, it’s an inexpensive drug with a broad spectrum of activity and decades of safety, to the extent that it may be even fruitful to examine it for both long COVID and for those suffering from vaccine adverse reactions.
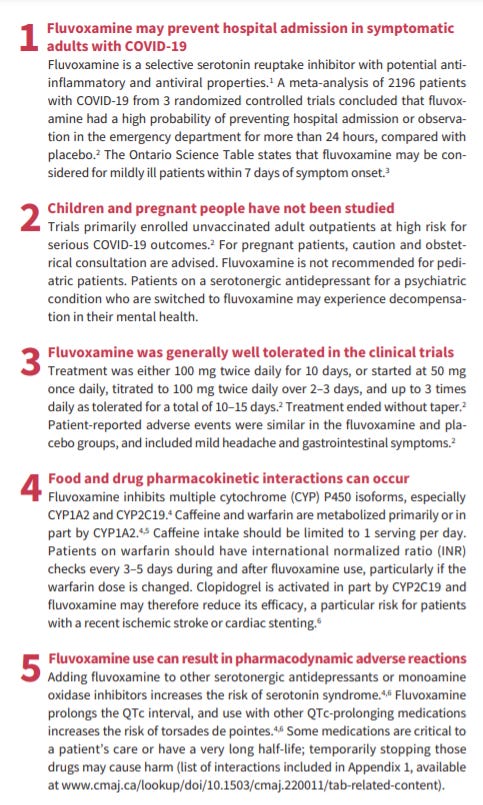
I’ll end this entire series with one more additional post that helps to summarize a few of the key points with Fluvoxamine (Wu et. al.):
One thing to point out is Point 2. Like with most clinical trials participants under 18 and pregnant women are excluded. However, because Fluvoxamine has been prescribed for decades there should be well established evidence of its safety in children. Yes, Fluvoxamine is prescribed to children, and even pregnant women. If someone chooses to discuss Fluvoxamine with medical professionals, care should be taken to look at Point 4 and discuss possible contraindications with medications already in use.
So with that I’ll collect all of the prior Fluvoxamine posts and will include citations below. Note that my citations focus solely on science articles and papers. If readers prefer I include all of the articles I link to please let me know.
Fluvoxamine- The Little SSRI that Could
Part I: Brief Overview, Tortuous History, and MOAs
Like with all posts the first part introduces Fluvoxamine, providing a brief history into it’s structure and development. I also briefly discuss the emerging concerns over SSRIs through the context of Fluvoxamine’s relationship to the Columbine Shooting Massacre. Lastly, I discuss some of Fluvoxamine’s mechanisms of action.
Part II: Nonclinical Examination of Lysosomotropism and the ASM/Ceramide Pathway
Going more in depth I then examine each MOA in further detail. Based on my research I found it important to discuss Lysosomotropism and the ASM/Ceramide pathway, although I decided to skip over discussing some of these MOAs in Part I, and therefore included it here. I then provide studies from the literature involving these pathways, and include studies involving these pathways, Fluvoxamine (or Fluoxetine) and SARS-COV2 infection.
Part III: Nonclinical Examination of Fluvoxamine, Sigma-1 Agonism and ER Stress
Just like Part II this post goes deeper into the last MOA being examined. It’s probably one of the most important due to the role ER Stress plays in many diseases including diabetes, cardiovascular disease, and neurodegeneration just to name a few. Although there’s no studies providing a causal link between Fluvoxamine, S1R receptors, ER Stress, and SARS-COV2 infection the information provided allows for as close of an examination as possible.
Part IV: Nonclinical Examination of Fluoxetine/Fluvoxamine & Emerging Clinical Trial Results
Finally, we take a look at clinical trials involving Fluvoxamine, including the well-known TOGETHER trial. Beforehand, I provide two more in vitro assays suggesting that both Fluvoxamine and Fluoxetine are effective in reducing SARS-COV2 infection. Overall, the results all suggest that Fluvoxamine should be an effective therapeutic agent for fighting COVID.
A Proposed "Pseudo-infection" Hypothesis
Research into Fluvoxamine led me to think about parallels between the vaccines and COVID infection. Although the original hypothesis wanted to examine the vaccines through their role in inducing ER Stress, I changed my hypothesis to examine the vaccination process through the lens of a “pseudoinfection”, addressing the importance of examining all aspects of the vaccines in order to gain a better understanding about these adverse reactions.
Note: The Citations will make this post too long and so I will post it separately and link it here. Apologies for the inconvenience!
Citations
Chu, A. & Wadhwa, R. Selective serotonin reuptake inhibitors. StatPearls [Internet]. Available at: https://www.ncbi.nlm.nih.gov/books/NBK554406/.
Marčec, R., & Likić, R. (2021). Could fluvoxamine keep COVID-19 patients out of hospitals and intensive care units?. Croatian medical journal, 62(1), 95–100. https://doi.org/10.3325/cmj.2021.62.95
Lenze, E. J., Mattar, C., Zorumski, C. F., Stevens, A., Schweiger, J., Nicol, G. E., Miller, J. P., Yang, L., Yingling, M., Avidan, M. S., & Reiersen, A. M. (2020). Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19: A Randomized Clinical Trial. JAMA, 324(22), 2292–2300. https://doi.org/10.1001/jama.2020.22760
Rosen, D. A., Seki, S. M., Fernández-Castañeda, A., Beiter, R. M., Eccles, J. D., Woodfolk, J. A., & Gaultier, A. (2019). Modulation of the sigma-1 receptor-IRE1 pathway is beneficial in preclinical models of inflammation and sepsis. Science translational medicine, 11(478), eaau5266. https://doi.org/10.1126/scitranslmed.aau5266
Seftel, D., & Boulware, D. R. (2021). Prospective Cohort of Fluvoxamine for Early Treatment of Coronavirus Disease 19. Open forum infectious diseases, 8(2), ofab050. https://doi.org/10.1093/ofid/ofab050
Fluvoxamine. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Available at: https://www.ncbi.nlm.nih.gov/books/NBK548905/.
Sukhatme, V. P., Reiersen, A. M., Vayttaden, S. J., & Sukhatme, V. V. (2021). Fluvoxamine: A Review of Its Mechanism of Action and Its Role in COVID-19. Frontiers in pharmacology, 12, 652688. https://doi.org/10.3389/fphar.2021.652688
Sansone, R. A., & Sansone, L. A. (2014). Serotonin norepinephrine reuptake inhibitors: a pharmacological comparison. Innovations in clinical neuroscience, 11(3-4), 37–42.
Hashimoto, Y., Suzuki, T., & Hashimoto, K. (2022). Mechanisms of action of fluvoxamine for COVID-19: a historical review. Molecular psychiatry, 1–10. Advance online publication. https://doi.org/10.1038/s41380-021-01432-3
Maurice, T., & Su, T. P. (2009). The pharmacology of sigma-1 receptors. Pharmacology & therapeutics, 124(2), 195–206. https://doi.org/10.1016/j.pharmthera.2009.07.001
Alberts, B. The endoplasmic reticulum. Molecular Biology of the Cell. 4th edition. Available at: https://www.ncbi.nlm.nih.gov/books/NBK26841/.
Read, A., & Schröder, M. (2021). The Unfolded Protein Response: An Overview. Biology, 10(5), 384. https://doi.org/10.3390/biology10050384
Xue, M., & Feng, L. (2021). The Role of Unfolded Protein Response in Coronavirus Infection and Its Implications for Drug Design. Frontiers in microbiology, 12, 808593. https://doi.org/10.3389/fmicb.2021.808593
Shi, M., Chen, F., Chen, Z., Yang, W., Yue, S., Zhang, J., & Chen, X. (2021). Sigma-1 Receptor: A Potential Therapeutic Target for Traumatic Brain Injury. Frontiers in cellular neuroscience, 15, 685201. https://doi.org/10.3389/fncel.2021.685201
Krystel-Whittemore, M., Dileepan, K. N., & Wood, J. G. (2016). Mast Cell: A Multi-Functional Master Cell. Frontiers in immunology, 6, 620. https://doi.org/10.3389/fimmu.2015.00620
Zhou, Z., Ren, L., Zhang, L., Zhong, J., Xiao, Y., Jia, Z., Guo, L., Yang, J., Wang, C., Jiang, S., Yang, D., Zhang, G., Li, H., Chen, F., Xu, Y., Chen, M., Gao, Z., Yang, J., Dong, J., Liu, B., … Wang, J. (2020). Heightened Innate Immune Responses in the Respiratory Tract of COVID-19 Patients. Cell host & microbe, 27(6), 883–890.e2. https://doi.org/10.1016/j.chom.2020.04.017
Chen, Z. H., Xiao, L., Chen, J. H., Luo, H. S., Wang, G. H., Huang, Y. L., & Wang, X. P. (2008). Effects of fluoxetine on mast cell morphology and protease-1 expression in gastric antrum in a rat model of depression. World journal of gastroenterology, 14(45), 6993–6998. https://doi.org/10.3748/wjg.14.6993
Dai, H., & Korthuis, R. J. (2011). Mast Cell Proteases and Inflammation. Drug discovery today. Disease models, 8(1), 47–55. https://doi.org/10.1016/j.ddmod.2011.06.004
Blaess, M., Kaiser, L., Sommerfeld, O., Csuk, R., & Deigner, H. P. (2021). Drugs, Metabolites, and Lung Accumulating Small Lysosomotropic Molecules: Multiple Targeting Impedes SARS-CoV-2 Infection and Progress to COVID-19. International journal of molecular sciences, 22(4), 1797. https://doi.org/10.3390/ijms22041797
Glebov O. O. (2021). Low-Dose Fluvoxamine Modulates Endocytic Trafficking of SARS-CoV-2 Spike Protein: A Potential Mechanism for Anti-COVID-19 Protection by Antidepressants. Frontiers in pharmacology, 12, 787261. https://doi.org/10.3389/fphar.2021.787261
Breiden, B., & Sandhoff, K. (2021). Acid Sphingomyelinase, a Lysosomal and Secretory Phospholipase C, Is Key for Cellular Phospholipid Catabolism. International journal of molecular sciences, 22(16), 9001. https://doi.org/10.3390/ijms22169001
Kornhuber, J., Hoertel, N., & Gulbins, E. (2021). The acid sphingomyelinase/ceramide system in COVID-19. Molecular psychiatry, 1–8. Advance online publication. https://doi.org/10.1038/s41380-021-01309-5
Carpinteiro, A., Edwards, M. J., Hoffmann, M., Kochs, G., Gripp, B., Weigang, S., Adams, C., Carpinteiro, E., Gulbins, A., Keitsch, S., Sehl, C., Soddemann, M., Wilker, B., Kamler, M., Bertsch, T., Lang, K. S., Patel, S., Wilson, G. C., Walter, S., Hengel, H., … Gulbins, E. (2020). Pharmacological Inhibition of Acid Sphingomyelinase Prevents Uptake of SARS-CoV-2 by Epithelial Cells. Cell reports. Medicine, 1(8), 100142. https://doi.org/10.1016/j.xcrm.2020.100142
Shu, H., Peng, Y., Hang, W., Li, N., Zhou, N., & Wang, D. W. (2022). Emerging Roles of Ceramide in Cardiovascular Diseases. Aging and disease, 13(1), 232–245. https://doi.org/10.14336/AD.2021.0710
Abdullah, C. S., Alam, S., Aishwarya, R., Miriyala, S., Panchatcharam, M., Bhuiyan, M., Peretik, J. M., Orr, A. W., James, J., Osinska, H., Robbins, J., Lorenz, J. N., & Bhuiyan, M. S. (2018). Cardiac Dysfunction in the Sigma 1 Receptor Knockout Mouse Associated With Impaired Mitochondrial Dynamics and Bioenergetics. Journal of the American Heart Association, 7(20), e009775. https://doi.org/10.1161/JAHA.118.009775
Almanza, A., Carlesso, A., Chintha, C., Creedican, S., Doultsinos, D., Leuzzi, B., Luís, A., McCarthy, N., Montibeller, L., More, S., Papaioannou, A., Püschel, F., Sassano, M. L., Skoko, J., Agostinis, P., de Belleroche, J., Eriksson, L. A., Fulda, S., Gorman, A. M., Healy, S., … Samali, A. (2019). Endoplasmic reticulum stress signalling - from basic mechanisms to clinical applications. The FEBS journal, 286(2), 241–278. https://doi.org/10.1111/febs.14608
Köseler, A., Sabirli, R., Gören, T., Türkçüer, I., & Kurt, Ö. (2020). Endoplasmic Reticulum Stress Markers in SARS-COV-2 Infection and Pneumonia: Case-Control Study. In vivo (Athens, Greece), 34(3 Suppl), 1645–1650. https://doi.org/10.21873/invivo.11956
Hong, J., Kim, K., Kim, J. H., & Park, Y. (2017). The Role of Endoplasmic Reticulum Stress in Cardiovascular Disease and Exercise. International journal of vascular medicine, 2017, 2049217. https://doi.org/10.1155/2017/2049217
Hosoi, T., Miyahara, T., Kayano, T., Yokoyama, S., & Ozawa, K. (2012). Fluvoxamine attenuated endoplasmic reticulum stress-induced leptin resistance. Frontiers in endocrinology, 3, 12. https://doi.org/10.3389/fendo.2012.00012
Lin, J. H., Walter, P., & Yen, T. S. (2008). Endoplasmic reticulum stress in disease pathogenesis. Annual review of pathology, 3, 399–425. https://doi.org/10.1146/annurev.pathmechdis.3.121806.151434
Omi, T., Tanimukai, H., Kanayama, D., Sakagami, Y., Tagami, S., Okochi, M., Morihara, T., Sato, M., Yanagida, K., Kitasyoji, A., Hara, H., Imaizumi, K., Maurice, T., Chevallier, N., Marchal, S., Takeda, M., & Kudo, T. (2014). Fluvoxamine alleviates ER stress via induction of Sigma-1 receptor. Cell death & disease, 5(7), e1332. https://doi.org/10.1038/cddis.2014.301
DeSai, C. & Shapshak, A. Cerebral ischemia. StatPearls [Internet]. Available at: https://www.ncbi.nlm.nih.gov/books/NBK560510/.
Koçak Tufan, Z., Kayaaslan, B., & Mer, M. (2021). COVID-19 and Sepsis. Turkish journal of medical sciences, 51(SI-1), 3301–3311. https://doi.org/10.3906/sag-2108-239
Echavarría-Consuegra, L., Cook, G. M., Busnadiego, I., Lefèvre, C., Keep, S., Brown, K., Doyle, N., Dowgier, G., Franaszek, K., Moore, N. A., Siddell, S. G., Bickerton, E., Hale, B. G., Firth, A. E., Brierley, I., & Irigoyen, N. (2021). Manipulation of the unfolded protein response: A pharmacological strategy against coronavirus infection. PLoS pathogens, 17(6), e1009644. https://doi.org/10.1371/journal.ppat.1009644
Chan, C. P., Siu, K. L., Chin, K. T., Yuen, K. Y., Zheng, B., & Jin, D. Y. (2006). Modulation of the unfolded protein response by the severe acute respiratory syndrome coronavirus spike protein. Journal of virology, 80(18), 9279–9287. https://doi.org/10.1128/JVI.00659-06
Rhea, E. M., Logsdon, A. F., Hansen, K. M., Williams, L. M., Reed, M. J., Baumann, K. K., Holden, S. J., Raber, J., Banks, W. A., & Erickson, M. A. (2021). The S1 protein of SARS-CoV-2 crosses the blood-brain barrier in mice. Nature neuroscience, 24(3), 368–378. https://doi.org/10.1038/s41593-020-00771-8
Hsu, A. C.-Y. et al. SARS-COV-2 spike protein promotes hyper-inflammatory response that can be ameliorated by spike-antagonistic peptide and FDA-approved ER stress and MAP kinase inhibitors in vitro. bioRxiv Available at: https://www.biorxiv.org/content/10.1101/2020.09.30.317818v1.full.
Zimniak, M., Kirschner, L., Hilpert, H. et al. The serotonin reuptake inhibitor Fluoxetine inhibits SARS-CoV-2 in human lung tissue. Sci Rep 11, 5890 (2021). https://doi.org/10.1038/s41598-021-85049-0
Hillhouse, T. M., & Porter, J. H. (2015). A brief history of the development of antidepressant drugs: from monoamines to glutamate. Experimental and clinical psychopharmacology, 23(1), 1–21. https://doi.org/10.1037/a0038550
Fred, S. M., Kuivanen, S., Ugurlu, H., Casarotto, P. C., Levanov, L., Saksela, K., Vapalahti, O., & Castrén, E. (2022). Antidepressant and Antipsychotic Drugs Reduce Viral Infection by SARS-CoV-2 and Fluoxetine Shows Antiviral Activity Against the Novel Variants in vitro. Frontiers in pharmacology, 12, 755600. https://doi.org/10.3389/fphar.2021.755600
Reis G, Dos Santos Moreira-Silva EA, Silva DCM, et al. Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial. Lancet Glob Health. 2022;10(1):e42-e51. doi:10.1016/S2214-109X(21)00448-4
Calusic, M., Marcec, R., Luksa, L., Jurkovic, I., Kovac, N., Mihaljevic, S., & Likic, R. (2021). Safety and efficacy of fluvoxamine in COVID-19 ICU patients: An open label, prospective cohort trial with matched controls. British journal of clinical pharmacology, 10.1111/bcp.15126. Advance online publication. https://doi.org/10.1111/bcp.15126
Hoertel, N., Sánchez-Rico, M., Vernet, R. et al. Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study. Mol Psychiatry 26, 5199–5212 (2021). https://doi.org/10.1038/s41380-021-01021-4
Kremsner PG, Ahuad Guerrero RA, Arana-Arri E, et al. Efficacy and safety of the CVnCoV SARS-CoV-2 mRNA vaccine candidate in ten countries in Europe and Latin America (HERALD): a randomised, observer-blinded, placebo-controlled, phase 2b/3 trial [published online ahead of print, 2021 Nov 23]. Lancet Infect Dis. 2021;22(3):329-340. doi:10.1016/S1473-3099(21)00677-0
Röltgen, K., Nielsen, S., Silva, O., Younes, S. F., Zaslavsky, M., Costales, C., Yang, F., Wirz, O. F., Solis, D., Hoh, R. A., Wang, A., Arunachalam, P. S., Colburg, D., Zhao, S., Haraguchi, E., Lee, A. S., Shah, M. M., Manohar, M., Chang, I., Gao, F., … Boyd, S. D. (2022). Immune imprinting, breadth of variant recognition, and germinal center response in human SARS-CoV-2 infection and vaccination. Cell, S0092-8674(22)00076-9. Advance online publication. https://doi.org/10.1016/j.cell.2022.01.018
He, B. Viruses, endoplasmic reticulum stress, and interferon responses. Cell Death Differ 13, 393–403 (2006). https://doi.org/10.1038/sj.cdd.4401833
Fung, T. S., & Liu, D. X. (2014). Coronavirus infection, ER stress, apoptosis and innate immunity. Frontiers in microbiology, 5, 296. https://doi.org/10.3389/fmicb.2014.00296
Li, S., Kong, L., & Yu, X. (2015). The expanding roles of endoplasmic reticulum stress in virus replication and pathogenesis. Critical reviews in microbiology, 41(2), 150–164. https://doi.org/10.3109/1040841X.2013.813899
Hong, J., Kim, K., Kim, J. H., & Park, Y. (2017). The Role of Endoplasmic Reticulum Stress in Cardiovascular Disease and Exercise. International journal of vascular medicine, 2017, 2049217. https://doi.org/10.1155/2017/2049217
Zha, X., Yue, Y., Dong, N. & Xiong, S. Endoplasmic Reticulum Stress Aggravates Viral Myocarditis by Raising Inflammation Through the IRE1-Associated NF-κB Pathway. Canadian Journal of Cardiology Available at: https://www.onlinecjc.ca/article/S0828-282X(15)00178-6/fulltext.
Zhang, H., Yue, Y., Sun, T., Wu, X., & Xiong, S. (2017). Transmissible endoplasmic reticulum stress from myocardiocytes to macrophages is pivotal for the pathogenesis of CVB3-induced viral myocarditis. Scientific reports, 7, 42162. https://doi.org/10.1038/srep42162
Luo, T., Kim, J. K., Chen, B., Abdel-Latif, A., Kitakaze, M., & Yan, L. (2015). Attenuation of ER stress prevents post-infarction-induced cardiac rupture and remodeling by modulating both cardiac apoptosis and fibrosis. Chemico-biological interactions, 225, 90–98. https://doi.org/10.1016/j.cbi.2014.10.032
Oster ME, Shay DK, Su JR, et al. Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021. JAMA. 2022;327(4):331–340. doi:10.1001/jama.2021.24110
Rao, R. V., & Bredesen, D. E. (2004). Misfolded proteins, endoplasmic reticulum stress and neurodegeneration. Current opinion in cell biology, 16(6), 653–662. https://doi.org/10.1016/j.ceb.2004.09.012
Prasanth, M. I., Malar, D. S., Tencomnao, T. & Brimson, J. M. The emerging role of the sigma-1 receptor in autophagy: Hand-in-hand targets for the treatment of alzheimer's. Taylor & Francis Available at: https://www.tandfonline.com/doi/full/10.1080/14728222.2021.1939681?scroll=top&needAccess=true.
Jin, J. L., Fang, M., Zhao, Y. X., & Liu, X. Y. (2015). Roles of sigma-1 receptors in Alzheimer's disease. International journal of clinical and experimental medicine, 8(4), 4808–4820.
Song, W. J., Hui, C., Hull, J. H., Birring, S. S., McGarvey, L., Mazzone, S. B., & Chung, K. F. (2021). Confronting COVID-19-associated cough and the post-COVID syndrome: role of viral neurotropism, neuroinflammation, and neuroimmune responses. The Lancet. Respiratory medicine, 9(5), 533–544. https://doi.org/10.1016/S2213-2600(21)00125-9
Wu, P. E., Austin, E. & Leong, D. Fluvoxamine for symptomatic outpatients with covid-19. CMAJ Available at: https://www.cmaj.ca/content/194/7/E258.





Thank you for your thorough report on Fluvoxamine and for putting all your posts into a single experience so they can be more easily accessed. Your work and wonderful explanations are deeply appreciate.