Myocarditis from Vaccines or COVID
And why we apparently still don’t have reliable evidence about either.
Last week The Naked Emperor covered a new article detailing the rate of myocarditis and pericarditis among Scandinavian countries. As of this day we still do not know the root cause of vaccination and myocarditis. We certainly know that there is a lot of disingenuous discussions that are downplaying their actual prevalence.
Based on this I wanted to look at this study for myself. However, instead of looking at the study I wanted to point to a few interesting aspects that were glossed over by the researchers and why these would be important.
Heart Tissues- a Mini Overview
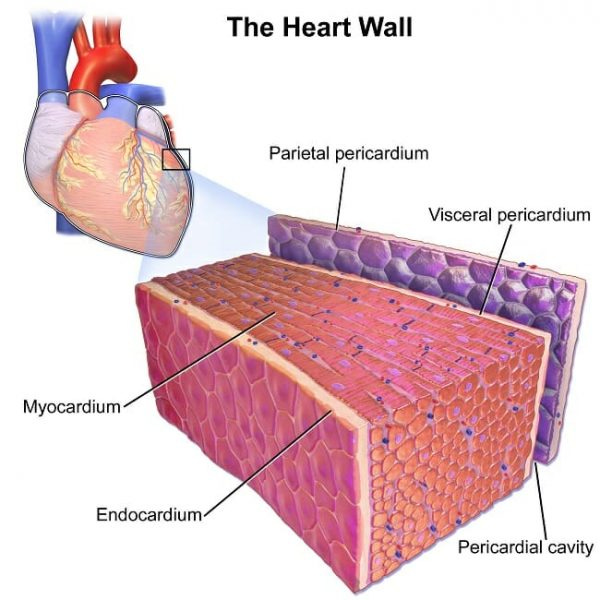
To start, let’s look at the anatomy of the heart and get a little examination into the differences between myocarditis and pericarditis. I’m sure many people have heard a little about the two but may not know the difference, so it may be worth providing a little explanation as to what these tissues are.
To provide a brief overview, the heart is comprised of several tissue layers:
The pericardium is the outermost tissue of the heart and is comprised of two layers separated by fluid, essentially creating a sac-like surrounding around the heart. The main function of the pericardium is to serve as a protective buffer between the heart and other external structures by reducing friction that may occur when the heart pumps blood.
Pericarditis is inflammation of these two layers of pericardium. Inflammation may lead to constriction of these layers that puts pressure on the heart. It can also cause the layers to rub together and cause scarring and tissue damage of the heart as well.
The myocardium, with the Greek suffix myo- tells us what this layer of tissue is comprised of- muscles. This layer serves as the muscle of the heart and provides it with the contractility needed to pump blood. Because it is comprised of muscle fibers, this layer of tissue requires a lot of energy and thus is comprised of many mitochondria and engages in a lot of metabolic activities.
Myocarditis is inflammation of these muscle, which may alter the heart’s ability to pump blood resulting in cardiac arrhythmia and other irregularities.
Although not discussed, we can go over the endocardium as well. The endocardium is the innermost tissue layer of the heart, and its makeup closely resembles that of the inner lining of our blood vessels.
A few terms of (scientific) endearment
Before going into a few interesting points in the article I want to define a few terms so that you can better understand the paper and tackle it on your own.
The figures and paper mentions the term “exposed” and “unexposed” several times. These are artifacts of the methodology- all they really refer to are “vaccinated” and “unvaccinated” groups so don’t be confused when seeing those terms in the JAMA paper.
The paper also refers to a number called “Person years”, and it’s somewhat related to the concept of light years, which refers to the distance light travels in a year.
Person years refer to how many incidences are expected to occur over the course of a year. Let’s say that one study occurred over the course of a month, and within that month a population of 100 people experienced 15 incidences (whatever variable was being measured, such as cancer rates or some diagnosis of a disease). A person year would take that value and extrapolate it over an entire year (15*12) and get 180 incidences in a 100 person year. This JAMA study refers to a value of “1000 person years (PYR)” which just indicates how many incidences of myocarditis are likely to occur over the course of a year when examining 1000 people. Following our example, we would multiply both values by 10 which would give us 1,800 incidences per 1000 person years.
Although this is a standard statistical methodology, we can see some faults with this type of measurement as it makes several assumptions in heterogeneity of participants and may broadly generalize based on the duration of the study.
The IRR refers to the Incidence-Rate Ratio, and just like the name implies it refers to the ratio of the experimental incidence rate compared to a control. It’s calculation is based on the reference- in this case the unvaccinated group which is considered a representation for the rate of myocarditis/pericarditis that should be expected in the general population sans vaccines. It takes the number of incidences and divides it by the number of participants over a set time period to provide an incidence rate (IR).
IR = measured incidences/(participants*timeframe)
Then, it takes the incidence rate of the vaccinated and divides it by the incidence rate of the unvaccinated:
(IR vaxxed/ IR unvaxxed) = IRR
What’s important with this value is that it provides a value relative to the control and indicates whether the rates of myocarditis/pericarditis are above the control’s baseline.
IRR values greater than 1 would indicate a greater incidence of heart inflammation than should be expected while a value less than 1 would indicate that rates of heart inflammation among the vaccinated are lower than would be expected. What’s important here is to understand that an IRR value lower than 1 doesn’t indicate that these vaccines are somehow protective- be careful of making that extrapolation.
For more on Incidence measurements, refer to this article.
Points Worth Examining
The paper in question is the recent JAMA paper titled SARS-CoV-2 Vaccination and Myocarditis in a Nordic Cohort Study of 23 Million Residents.
Like I stated before, I believe the Naked Emperor provided a good brief rundown of the study and I refer you to that post.
This paper is also a fairly straightforward read and so it doesn’t require a lot of prior experience to examine, although the defined terms should provide some help.
So instead I am going to point out a few things that I find are interesting, and requires further examination.
What’s going on with Heterologous Vaccination?
When comparing rates of myocarditis between Pfizer and Moderna it’s true that Moderna appears to have the greatest rates of myocarditis and pericarditis. However, this appears to only apply to homologous vaccination- when somoene is given the same type of vaccine. What’s strange is that heterologous vaccination, which is a mixing of different vaccines (notably Pfizer and Moderna), appears to have the greatest level of heart inflammation.
However, the researchers apparently glossed over this alarming finding:
This is the only time where this is mentioned in the article, and yet it has one of the highest IRR values in the study. Why the researchers didn’t quite elaborate on this finding is questionable, as it would at least indicate something more than dosing could be occurring.
Unfortunately, the researchers do not differentiate between whether the first dose was Pfizer or if the first dose was Moderna.
Although I do not like to assume, what I believe may have happened was that some patients received Moderna as their first dose and experienced an adverse reaction. This adverse reaction likely led to a recommendation of using Pfizer- we have evidence of doctors suggesting that already. Afterwards, it could be that the second dose of an mRNA vaccine led to another adverse event, possibly myocarditis/pericarditis.
These results at least point to something more going on that just dosing. It could be likely that these people are at higher risk of experiencing adverse events.
It could also point to concerns over formulation. For all intents and purposes, both mRNA vaccines should only differ in the lipid nanoparticles. As I have written previously, there may be concerns that these LNPs may be recognized by the body and transported based on the recognized structure (i.e. if they look like LDL and move to where cholesterol is used by the body). There may be questions as to whether different LNP formations may mimic different lipid structures in the body, although again this is just more speculation.
Nonetheless, why these researchers did not differentiate between the dosing regimens means that we may be overlooking something critical to the safety of these vaccines.
The Importance of Relativity
If we take a look at the discussion section we will notice an interesting comment made by the researchers (emphasis mine):
Myocarditis after mRNA vaccination was rare in this study cohort and even among young males. The risk of myocarditis following the mRNA vaccines has been evaluated by the US Food and Drug Administration, which concluded that the benefits of vaccination outweigh the risks and fully authorized the use of mRNA-1273 in persons 18 years or older and BNT162b2 in persons 16 years or older. In addition, BNT162b2 is authorized for emergency use in children 5 years or older.20,21 The European Medicines Agency concluded that the benefits of vaccination outweigh the risks and approved mRNA-1273 for use in persons 12 years or older and BNT162b2 for those 5 years or older.22,23 In addition, a comment published by the American College of Cardiology24 evaluated vaccine-associated myocarditis risk and concluded that the benefits of vaccination outweigh the risks. As of January 2022, there have been nearly 5.8 million deaths associated with COVID-19 worldwide since the start of the pandemic.25 All currently available SARS-CoV-2 mRNA vaccines are highly effective against severe COVID-19 and provide some protection against transmission and infection.26-28 There is some evidence that the mRNA-1273 vaccine, possibly owing to its higher concentration of mRNA, is associated with increased immunogenicity and effectiveness.29,30 This more profound immune response could be one reason for the higher risk of myocarditis, but this hypothesis needs to be investigated further.
The first line is interesting, as it glosses over the main concerns with these vaccines. As I have continuously mentioned, studies are relative- they are based on the control group and are evaluated under these circumstances. Even in this study age-stratified and sex-stratified data suggest that the rates of both myocarditis and pericarditis are higher than would be expected in the general population, especially among those who are younger.
I would actually argue this point is redundant- we already know that these vaccines are likely to lead to rates of heart inflammation.
What’s more important is to see what the rates of myocarditis/pericarditis are from a COVID infection, and we can compare that data to the rate among vaccinated individuals.
If we look at eTable 7 from the supplemental material we can see the rates of myocarditis among young men are fairly low and increased with age. More importantly, rates of myocarditis among young men between the ages of 12-15 were zero:
Now, we do have to be careful as the IRR is affected by the “no infection” control group. Since this group is different than the control group used in the vaccine calculations they may not be directly related, but they do provide some correlative evidence of some relationship. On this basis, what we can see is that rates of myocarditis were higher among young men (12-24) who were vaccinated compared to young men who were infected with COVID.
*For example, the IRR for Males 16-24 who were diagnosed with myocarditis from a SARS-COV2 infection were 2.99 while the IRR for the 2nd dose of Pfizer and Moderna in this same group is 5.31 and 13.83, respectively.
Again, the researchers did not explain these results. Actually, these results run counter to what they described in their discussion, which states that the benefits of vaccinations outweigh the risks. What then, do we make of these results which would at least discredit this argument and instead suggests that the risk of myocarditis from vaccination are higher than infection for young men?
It would at least warrant further investigation, but it would also indicate that these vaccines aren’t “safe and effective”. We may even argue that “relatively safe and effective” would be hard to assess- the evidence at least disproves that much.
*Section added for context and clarity.
We Need More Evidence
For all it’s worth, the JAMA study brought to light many of the concerns we all have. However, this may run a little hollow for some of us. We already knew that rates of myocarditis were higher among the young, and so this study only validates something we already knew. It’s a little disingenuous for the media to report on it after millions of adolescents were vaccinated; there’s no take-backs with these vaccines.
But what’s interesting is how these researchers apparently glossed over a few concerning points. Why are there such high rates of myocarditis and pericarditis in heterologous vaccine recipients? Does this raise questions about dosing being the main concern, or does it indicate individual differences as a large contributor to adverse reactions, such that people already at risk for myocarditis were told to use Pfizer rather than Moderna for their 2nd dose? None of these questions were answered by the researchers, and yet the data is there to analyze and provide some much needed context.
The CDC approved of the idea of mix-and-match vaccines in October 2021 with respect to boosters, but it appears that there may be concerns for even mixing the mRNA vaccines. Again, as of now there really isn’t much evidence about the adverse effects of heterologous dosing.
The higher IRR of myocarditis in young men given vaccines versus infections also raises questions towards the argument that the benefits of vaccination are greater than the risk of infection. Clearly the evidence suggests otherwise, and again considering that the evidence is there why did the researchers not address these findings? If anything, I would argue that this provides for something else to research and analyze- if only further research was done before massive vaccination.
We need more evidence, and we also need more researchers to be genuine in their findings. How many studies will we come across that may suggest that rates of myocarditis are higher among young men, only to contradict themselves and state that these are rare incidences (remember, that “rarity” should be evaluated within the context of what was being measured). There’s an overwhelming pressure to provide evidence that falls along the established narrative, and unless we can do away with this we may not be able to fully figure out what is going on.