Have Monoclonal Antibodies Lost their Effectiveness? (Review)
Part III: Concluding Remarks and Citations
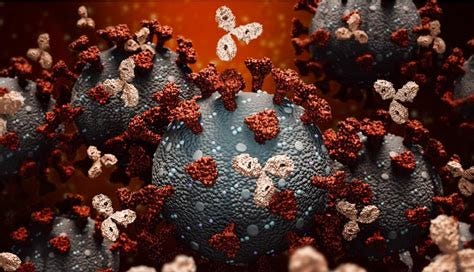
Monoclonals in the Era of Omicron
The questions as to whether monoclonal therapeutics will hold up to Omicron has caused a lot of controversies. In Dr. Malone’s recent interview with Joe Rogan, several questions were raised about the use of monoclonals. As Dr. Malone put it, many doctors are seeing that their hospitalizations are still being dominated by the Delta variant. Even then, many hospitals and medical centers are deciding to ban the use of monoclonals out of the notion that they are no longer effective, meaning that many patients will be left without a treatment option.
Other areas of the country are experiencing short supply and are wondering how to limit the little bit that they have. In such circumstances, the inability to discern a Delta infection from an Omicron infection may mean that vital monoclonals will be denied from people who may desperately need it while those who are more likely to experience mild symptoms may have monoclonals be wasted.
There’s several speculations for the short supply. Sotrovimab just recently began having broader distribution, and so supplies are likely to be limited by region. The shortage of Eli Lilly and Regeneron’s monoclonals are more questionable, with some reports suggesting that initial findings of lack of effectiveness halted many healthcare systems from the sourcing of these monoclonals specifically. This would be very concerning, as it would mean that the removal of therapeutics was based on assumptions and not lack of evidence. Again, even as Omicron gains prevalence, Delta is still persisting and should still be taken into consideration when examining treatment options.
A more nefarious reason for the lack of supplies would be one brought up by Dr. McCullough in his interview with Joe Rogan, in which he stated that the US government focused on an “all eggs in one basket” approach to COVID by focusing solely on vaccines and not therapeutics. This would greatly hinder both the funding and manufacturing of treatments, leading to both a shortage and delay of treatment options. There’s no full evidence to support this argument, although we have heard about plenty of monoclonal shortages starting all the way back into the summer months and continue to this day. This would also align with the strange demonization that monoclonals have been receiving among different social media circles. Even now comments have been made about the “experimental” nature of these monoclonals, even though most of these have been sourced through people with prior COVID infections.
We’ve outlined here that not all antibodies work alike, and that considerations should be made about which antibodies to use against which variant.
Eli Lilly’s monoclonals are the most likely to lose effectiveness as there is clear evidence of this already occurring with prior circulating variants. The use of two monoclonals with overlapping binding regions severely hindered these therapies, and it points to a flaw in methodology and R&D on the part of these manufacturers.
The evidence for Regeneron is slightly less clear cut. Molecular modeling suggests that Regeneron should still retain some effectiveness. However, all of the nonclinical trials we have examined suggest that Regeneron should lose most of its effectiveness. The development of two nonoverlapping antibodies would, in theory, work to reduce the odds of escape mutations arising as one deleterious mutation against one monoclonal should not affect the binding of the other monoclonal. Unfortunately, the unusually high number of spike protein mutations found in Omicron do not bode well for either of Regeneron’s monoclonals, suggesting that even the use of nonoverlapping antibodies may not prove effective in a scenario where a sudden emergence of a variant with many mutations proliferates and gains dominance.
Out of the 3 main monoclonals on the market, Sotrovimab is the most likely to still remain effective against Omicron. The studies examined here indicate a possible reduction, but the effectiveness should still persist. The sourcing of Sotrovimab highlights a unique perspective in the R&D of COVID monoclonals. Using the hypothesis that the most important spike protein regions for receptor binding should be the least likely to experience mutations, the researchers at GSK and Vir Biotechnology compared conserved spike regions of both SARS-COV and SARS-COV2. Using this information, they examined the antibodies from a survivor of the 2003 SARS-COV outbreak and screened for monoclonals with the characteristics listed here, eventually leading to the discovery of the parent antibody that would eventually lead to Sotrovimab.
The medical community is experiencing one of many crossroads. The question as to whether to stop providing monoclonals, or to find ways to discern between Delta and Omicron are causing rash decisions to be made that could drastically alter the course of this pandemic.
Poor policy planning is likely to have led to scarce resources which we are now paying for with rationing of supplies. It also doesn’t help that political pundits and social media influencers have weighed in on the monoclonal debate, going so far as to have Youtuber Ethan Klein recently denigrate Joe Rogan’s use of Regeneron to treat his COVID infection, even though this just showed Ethan’s ignorance to the subject he is so bold to criticize than anything of actual substance.
Rational, evidence-based science should be driving the policies surrounding monoclonal antibodies. Doctors who are concerned about whether to prescribe monoclonals may use PCR results as confirmation for variants. The “S Gene” drop found in many Omicron samples could be used to discern Omicron from Delta. Adding to this approach, many doctors prior to Omicron have already raised alarms about not being provided Ct values for their patients, so as an extension it would also make sense for doctors to raise concerns about receiving PCR results and examining them for lack of S Gene amplification.
Doctors also need to be sensible in their approach to Omicron. We have yet to find clear clinical evidence that Regeneron will lose effectiveness. Even so, the risk of prescribing Regeneron are minimal, with the worst outcome being that they have no effect against the virus. It’s disheartening to see many doctors operating off of suppositions that Regeneron will not work, when the fact of the matter is that it may be far more responsible to prescribe something that may not work rather than not prescribe anything and hope it doesn’t get worse. In some sense, many healthcare professionals are now treating monoclonal antibodies as many of the “drugs that shall not be named”. Remember, lack of evidence is not evidence of no effect, and doctors should do well to keep that idea in mind as they continue to practice medicine.
Monoclonal antibodies are one of the only therapeutics available to the public. Even though Molnupiravir and PAXLOVID have gained approval, the concerns over Molnupiravir’s possible mutagenicity still need to be addressed, and is likely to produce hesitancy over its use. PAXLOVID seems far more promising, although the initial rollout is likely to be far more limited compared to Molnupiravir. Even still, both of these therapeutics are not likely to reach the public for several more months, still leaving monoclonals as the only outpatient option.
The landscape of medicine has been shaken up by the onset of Omicron. Emerging evidence calls into question the neutralizing capabilities of vaccines, including boosters. Both vaccines and monoclonals operate off of the same principles, and if concerns are raised over monoclonal efficacy the same can be said for the vaccines in use today. This is leading to the ideas of providing Omicron-targeted vaccines and therapeutics gaining prevalence in the pharmaceutical realm. This raises questions about scenarios such as Original Antigenic Sin and Omicron-specific vaccines. OAS has yet to be fully elucidated, but the concerns are still warranted, especially if the antigenic distance between the wildtype virus and Omicron are too close to elicit “backboosting” of prior antibodies rather than brand new antibodies to target Omicron. As of now, Regeneron has indicated that they are developing “next generation” monoclonals that are able to target Omicron, and unlike vaccines monoclonals are less likely to run into concerns over OAS.
With emerging variants comes renewed concerns, but concerns should never override sensible, evidence-driven science. Science should drive the policies that we all must follow instead of following policies not based on any real evidence. Doctors and healthcare experts, by virtue of their education and practice, should do well to make sure that their decisions continue to remain rational and remain backed by science.
Citations
Brobst, B. Benefits and risks of administering monoclonal antibody therapy for coronavirus (COVID-19). StatPearls [Internet]. (2021). Available at: https://www.ncbi.nlm.nih.gov/books/NBK574507/
Hansen J, Baum A, Pascal KE, et al. Studies in humanized mice and convalescent humans yield a SARS-CoV-2 antibody cocktail. Science. 2020;369(6506):1010-1014. doi:10.1126/science.abd0827
Dougan M, Nirula A, Azizad M, et al. Bamlanivimab plus Etesevimab in Mild or Moderate Covid-19. N Engl J Med. 2021;385(15):1382-1392. doi:10.1056/NEJMoa2102685
Gupta, A. et al. Early treatment for covid-19 with SARS-COV-2 neutralizing antibody Sotrovimab: Nejm. New England Journal of Medicine Available at: https://www.nejm.org/doi/10.1056/NEJMoa2107934.
Dolgin E. 'Super-antibodies' could curb COVID-19 and help avert future pandemics [published correction appears in Nat Biotechnol. 2021 Jun 29;:]. Nat Biotechnol. 2021;39(7):783-785. doi:10.1038/s41587-021-00980-x
Chen J, Wang R, Gilby NB, Wei GW. Omicron (B.1.1.529): Infectivity, vaccine breakthrough, and antibody resistance. Preprint. ArXiv. 2021;arXiv:2112.01318v1. Published 2021 Dec 1.
Wilhelm, A. et al. Reduced neutralization of SARS-COV-2 omicron variant by vaccine Sera and monoclonal antibodies. medRxiv (2021). Available at: https://www.medrxiv.org/content/10.1101/2021.12.07.21267432v4.article-info.
Cao, Y. et al. Omicron escapes the majority of existing SARS-COV-2 neutralizing antibodies. BioRxiv (2021) Available at: https://www.biorxiv.org/content/10.1101/2021.12.07.470392v2.full.
VanBlargan, L. A. et al. An infectious SARS-COV-2 B.1.1.529 omicron virus escapes neutralization by several therapeutic monoclonal antibodies. bioRxiv (2021). Available at: https://www.biorxiv.org/content/10.1101/2021.12.15.472828v1.full.
Tada, T. et al. Increased resistance of SARS-COV-2 omicron variant to neutralization by vaccine-elicited and therapeutic antibodies. bioRxiv (2021). Available at: https://www.biorxiv.org/content/10.1101/2021.12.28.474369v1.full.



Using 3 targets for a PCR test with a stupid high cycle is bad enough.
With only 2 targets used how many more false positives will there be?
Thank you so much for this information